Short Report
Volume 3, Issue 7
Stent-Assisted Coil Embolization of MCA Bifurcation and Literature Review
Xiao-Dong Wang*
Inner Mongolia Autonomous Region General Hospital, Huhhot, China.
Corresponding Author :
Xiao-Dong Wang
Email: 302758945@qq.com
Received : May 28, 2024 Accepted : Jul 01, 2024 Published : Jul 08, 2024 Archived : www.meddiscoveries.org
Citation: Wang X. Stent-Assisted Coil Embolization of MCA Bifurcation and Literature Review. Med Discoveries. 2024; 3(7): 1181.
Copyright: © 2024 Wang X. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Coil embolization of aneurysms, after more than 20 years of clinical practice shows that several conditions must be met: 1. After the necessary interval, the entire aneurysm can achieve and maintain effective hemostasis. 2. Intra-aneurysm thrombosis is the result of intra-aneurysm hemostasis induced by the coil, which must take the necessary time to form a stable and organic coil thrombus complex; 3. The homogeneity and stability of the spring-thrombus complex at the base of the aneurysm must be sufficient to ensure neoendotheliosis and re-endothelialization of the aneurysm neck. Only if the above conditions are met can the operation be successful. The advantage of stent-assisted coil embolization is that the tumor bearing vessel can be preserved. However, since the foreign body is permanently placed in the main vessel, antiplatelet drugs need to be continued after surgery in order to prevent thrombus.
Clinical presentation and radiological studies
A 59-year-old man presented with dizziness with standing unsteady lasting for one week. The patient developed vertigo one week ago, aggravated when he switched positions to the left. Head CT showed: 1. Probable right occipital softening, 2. Multiple lacunar infarction and softening, 3. White matter osteoporosis. He was admitted to the cerebrovascular department to seek intracavascular treatment. The patient has a medical history of cerebral infarction two years ago, left vertebral artery stent implantation, left ear poor hearing. History of hypertension for more than ten years, up to 180/110 mmHg, the current drug control blood pressure. Neurological examination: Hearing loss in both ears, positive pathological signs on the left side, and positive signs of difficulty standing with closed eyes.
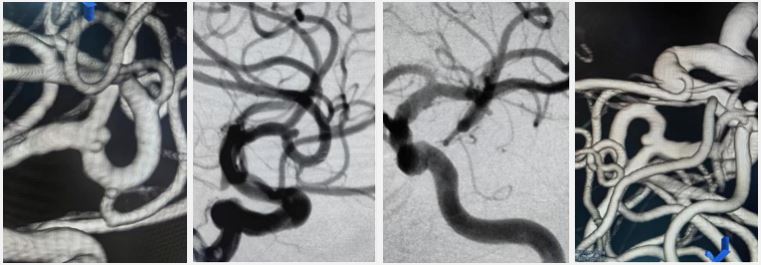
Cerebral angiography is arranged as soon as possible after the patient is admitted: After local anesthesia, right femoral artery puncture was performed, 5F arterial sheath was implanted, 5F pig tail catheter and single bend angiography catheter were sent under the guidance of 0.035 wire. Aortic arch, left and right carotid artery, and left and right vertebral artery angiography were performed, respectively, showing multiple aneurysms in the right middle cerebral artery and two aneurysms at the branch, 1.8 × 1.2 mm and 1.5 × 0.7 mm, respectively. Distal occlusion of the right vertebral artery V4 after left vertebral artery stenting in the ampulla of the right posterior communication segment (Figure 1).
Diagnosis: Symptomatic multiple aneurysms in the right middle cerebral artery.
Treatment: Under general anesthesia, Seldinger puncture was performed in the right femoral artery, a 6F arterial sheath was inserted, and a 6F guiding Catheter and a 5F multifunctional catheter (125 cm) was inserted to the C2 segment of the right internal carotid artery, followed by Y valve and double threeway catheter, one three-way receiving contrast agent, and one three-way receiving continuous pressure infusion of heparin saline. Angiography and 3D-DSA showed two aneurysms (1 × 1.1 mm, 1.6 × 1.7 mm) in the right middle cerebral artery. A microcatheter (SL-10) was inserted to the lower stem of M2 segment of the right middle cerebral artery at a selected working Angle, and the microcatheter was removed (Synchro 200), and the stent was implanted (Atlas) to cover the aneurysm neck, then remove the microcatheter, and take another microcatheter “Echelon 10” through the stent mesh guided by the microguide wire into the small aneurysm cavity, remove the microguide wire, and insert a spring diagram (prite 1+1) through the microcatheter for indentation. After the spring coil was recovered, the angiography showed the formation of intracranial thrombosis. The microcatheter was adjusted, and the catheter was sent to the larger aneurysm cavity through the stent mesh under the guidance of the microguide wire. The microguide wire was withdrawn, and two elastic yellow rings (prime 1.5 × 2) and the recovered elastic yellow map prime 1 + 1 were inserted successively. The angiography showed that the aneurysm was no longer developed, the right middle cerebral artery and the anterior cerebral artery branches were well developed, and all major blood vessels were well developed. The closure group was attached to the femoral puncture point, and the operation was successful. The tracheal intubation was removed after the operation, and the patient was conscious and returned to the ward safely.
Discussion
Endovascular techniques for the treatment of cerebral aneurysms provide a less invasive option than surgical clamping. Literature shows that spring-coil embolization of aneurysms at specific sites has a lower complication rate for patients with high-grade lesions. Advances in new technologies, such as three-dimensional spring-coil, balloon assisted remodeling, polymer embolization, stents and flow-guiding devices, and Pipeline embolization devices, etc. This allows vascular surgeons to treat previously untreatable lesions [1-3].
References
- Fernandez Bugzilla A, Guglielmi G, Viñuela F, Duckwiler GR. Endovascular occlusion of intracranial aneurysms with electrically detachable coils: correlation of aneurysm neck size and treatment results. AJNR Am J Neuroradiol. 1994; 15(5): 815-20. PMID: 8059647; PMCID: PMC8332188.
- Gobin YP, Viñuela F, Gurian JH, Guglielmi G, Duckwiler GR, et al. Treatment of large and giant fusiform intracranial aneurysms with Guglielmi detachable coils. J Neurosurg. 1996; 84(1): 55-62. doi: 10.3171/jns.1996.84.1.0055.
- Halbach VV, Higashida RT, Dowd CF, Fraser KW, Smith TP, et al. Endovascular treatment of vertebral artery dissections and pseudoaneurysms. J Neurosurg. 1993; 79(2): 183-91. doi: 10.3171/jns.1993.79.2.0183.