Research Article
Volume 3, Issue 6
Centralized Medical Observation in the COVID-19 Response: A Retrospective Field Study
Jian Jiang1,2*; Wenqing Rao1 ; Xuwei Tang1 ; Xiangju Hu1,3; Shuting Wu2
1Department of Epidemiology and Health Statistics, School of Public Health, Fujian Medical University, Fuzhou 350122, China.
2Medical Department, Fujian Provincial Hospital, Fuzhou 350001, China.
3Department of Endemic and Non-Communicable Diseases Prevention, Fujian Provincial Center for Disease Control and Prevention, Fuzhou 350012, China.
Corresponding Author :
Jian Jiang
Email: fjmu2002@fjmu.edu.cn
Received : May 17, 2024 Accepted : Jun 18, 2024 Published : Jun 25, 2024 Archived : www.meddiscoveries.org
Citation: Jiang J, Rao W, Tang X, Hu X, Wu S. Centralized Medical Observation in the COVID-19 Response: A Retrospective Field Study. Med Discoveries. 2024; 3(6): 1174.
Copyright: © 2024 Jiang J. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background: Non-drug interventions are the most active and effective response strategies until the availability of 100% effective vaccines and antiviral drugs. As one of the important means of non-drug interventions, centralized medical observation plays a crucial role in the epidemic prevention and control.
Methods: This retrospective study focused on the epidemic response in Putian city (Fujian, China) as the observation object, descriptive and qualitative analysis methods was discuss our practice and experience of the centralized medical observation during the epidemic response.
Results: In September 2021, a total of 205 confirmed cases and 41 asymptomatic patients were reported in Putian city; a total of 11,201 contacts of all types were tracked and all were included in centralized medical observation; 110 centralized medical observation sites were put into use; 3,173 staff of various types were selected and dispatched to centralized medical observation sites to undertake the task of the epidemic prevention and control.
Conclusion: Intensive medical observation assumes the tasks of isolation, health surveillance, nucleic acid testing, psychological assistance, infection prevention and control. It is an effective and practical strategy to deal with the epidemic of major infectious diseases caused by viruses transmitted via air or direct contact, such as the COVID-19.
Keywords: Centralized medical observation; COVID-19; Epidemic; Response; Non-drug interventions.
Introduction
The global spread of the COVID-19 has been in its third year since it was confirmed and declared by the World Health Organization, and it still deeply affects each of us [1-3]. With the Novel Coronavirus continuing to spread and mutate in the population, although some studies have showed that although the pathogenicity of the mutated virus is weakening, its infectivity is gradually increasing, and it is easier to evade vaccine-induced immunity [4-6]. In the face of this once-in-a-century major public health emergency, scientists from all over the world are still trying to find a way to completely defeat the virus. However, based on our experience, non-drug intervention is still the best strategy for us to prevent and control this epidemic until the availability of 100% effective vaccines and antiviral drugs[7-11].
With the characteristics such as being infectious in the incubation period, being difficult to identify patients with atypical symptoms, and a large number of infectious asymptomatic patients, the COVID-19 has a stronger transmission ability and is more difficult to control, compared with other infectious diseases [12-15]. According to the core principle of “early detection, early report, early isolation and early treatment” of infectious diseases, blocking the transmission chain as soon as possible is an effective magic weapon for us to curb the epidemic of infectious diseases [16-18]. When China responded to the first wave of the COVID-19 at home, it put forward the policy of “concentrating patients, experts, resources, and treatment”. At that time, in response to the challenges of a surge in the number of infections, medical resource panic squeeze and the serious shortage of hospital beds, Wuhan municipal government made use of public facilities such as stadiums to build 16 square makeshift hospitals. Which was used for the centralized treatment of Novel Coronavirus pneumonia patients with mild and asymptomatic symptoms [19,20]. This is the first time that the Chinese government has implemented a large-scale centralized medical observation to respond to the COVID-19, and it is also our great pioneering work in response to the epidemic of infectious diseases.
Centralized medical observation is an important part of nondrug interventions. It refers to a practice of isolating people, who may be at risk of transmission or those potentially infected in the incubation period who have not been found, in a designated site for medical observation in a single-room for no less than 14 days to cut off the transmission route, protect vulnerable groups and curb community transmission during the outbreak of infectious diseases [7,21,22]. Previously, a large number of studies have shown that isolation can effectively slow down and contain the epidemic [23-26]. Chinese scholars have also conducted preliminary discussions on centralized medical observation, but their studies either focus on the demographic characteristics of isolated populations, or the specific work in a certain aspect, such as infection prevention and control [27,28]. At present, in the epidemic prevention and control stage of “dynamic zero” in our country, in the face of local outbreaks of clustered epidemics, there is still a lack of general, systematic and comprehensive research on how to implement the centralized medical observation, how to strengthen comprehensive personnel management, how to ensure the implementation of measures and give full play to its role in epidemic prevention and control. Therefore, in this study, Putian city (Fujian, China) was taken as the observation object, and the retrospective analysis of the practice of centralized medical observation in response to clustered outbreaks was performed. Also, its role and management strategies in epidemic prevention and control were explored.
Objects and methods
This is a retrospective study based on the field observation. In September 2021, a clustered epidemic caused by the transmission of asymptomatic patients entering the country occurred in Putian city, Fujian, China. It lasted 15 days from the reporting of the first case on September 10 to the realization of “zero new cases” of community infections on September 25. In order to break the transmission chain and curb the spread of the epidemic as soon as possible, Putian implemented a largescale centralized medical observation.
The authors of this paper participated in the whole process of the epidemic prevention and control in Putian city, and collected the data and detailed information on the number of the infected during the epidemic, the number of people under centralized medical observation, the opening and using of sites, on-site staff, management modes and work process and so on. Based on the on-site observation of the epidemic response, the practice and management experience of centralized medical observation in Putian city were introduced and discussed.
The descriptive and qualitative analysis was performed on the collected data, and IBM SPSS 25 was applied to the standardized processing and statistical analysis of the data. Part of the data came from the epidemic information bulletin on the official website of the local governments, including Fujian Provincial Health Commission(http://wjw.fujian.gov.cn), Putian Municipal People’s Government (https://www.putian.gov.cn), Xiamen Municipal People’s Government (http://www.xm.gov. cn), Quanzhou Municipal People’s Government(http://www. quanzhou.gov.cn).
The need for approval was waived by the local ethical committees as data were reported anonymously, and all participants agreed to the study. During the data collection period, Putian City was in the secondary response stage of public health emergencies, and the written informed consent was waived, which belongs to the emergency management of public health incidents.
Results
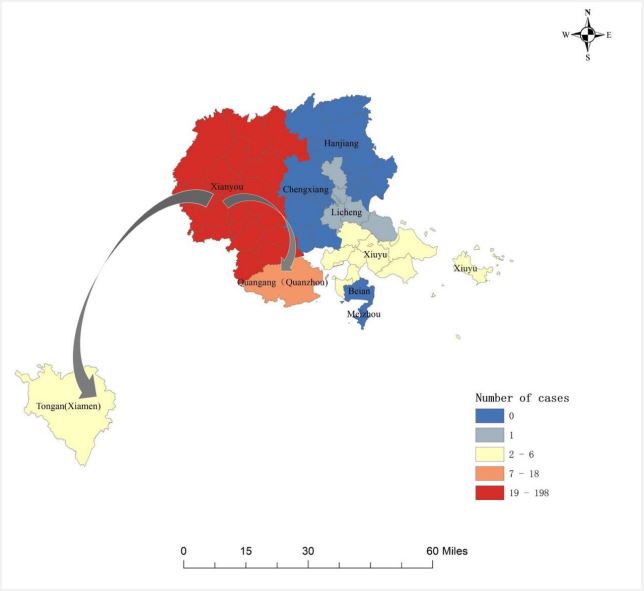
Putian is a coastal city in Fujian Province, China, under the jurisdiction of which are one county, four districts and two management committees (Xianyou County, Licheng District, Chengxiang District, Hanjiang District, Xiuyu District, Meizhou Island Management Committee and Beian Management Committee). According to the data of China’s seventh national census, Putian has a permanent resident population of 3,210,714 in 2020. Two students were found to be positive in nucleic acid testing during the regularly random sampling of the Novel Coronavirus in Xianyou County of Putian city, in September 2021. Having been reviewed by Putian municipal and Fujian provincial experts, the students were diagnosed as asymptomatic patients. After origin-tracing of viruses and gene sequencing, the virus was judged to come from a person who returned to Putian from abroad, belonging to the Delta variant strain of the Novel Coronavirus. Subsequently, the epidemic spread to the regions such as Licheng District (1 case), Xiuyu district (6 cases), Quangang District of Quanzhou City (18 cases) and Tong’an District of Xiamen City (6 cases). Owing to the rapid response, decisive decision-making and a series of non-drug interventions such as strict centralized medical observation, this round of epidemic in Putian city was basically controlled within an incubation period. Besides, most of the infected, with 198 confirmed cases and 41 asymptomatic patients, accounting for 97.15% of the total infected individuals in Putian, were controlled within Xianyou County, where the epidemic first occurred (Figure 1).
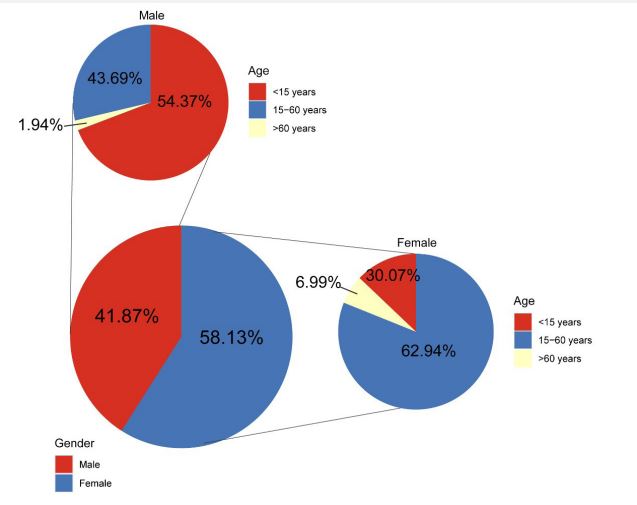
Since the first case was reported on September 10, 2021, a total of 205 confirmed cases and 41 asymptomatic patients were reported in this round of epidemics, of which 41.87% were male and 59.13% were female, and their ages ranged from 3 to 86 with an average age of 28.75 (SD=19.36). Their gender and age distribution are shown in Figure 2.
11,201 close contacts, sub-close contacts and space-time accompanying contacts (hereinafter referred to as “relevant individuals”) were screened and placed under the centralized medical observation. The peak of confirmed cases in a single day occurred on September 15 and the corresponding number of relevant individuals who were screened and placed under the centralized medical observation on that day was also the largest (1,687), and then began to decline. After September 25, no more new infected individuals were reported. The information on the confirmed cases, asymptomatic patients and relevant individuals in Putian from September 10 to September 25, 2021 is shown in Table 1.
As of September 25, 2021, a total of 198 confirmed cases and 41 asymptomatic patients have been reported in Xianyou, Putian City. At the same time, the epidemic has spilled over to Licheng District, Xiuyu District, Quangang District of Quanzhou City, and Tongan District of Xiamen City. (Source: Fujian Provincial Health Commission website, http://wjw.fujian.gov.cn, Putian People’s Government website, https://www.putian.gov.cn, Quanzhou People’s Government website, http://www.quanzhou.gov.cn, Xiamen People’s Government website, http://www.xm.gov.cn).
In the current round of epidemic in Putian city, there are 103 men and 143 women, 99 people under the age of 15, 134 people aged 15-60 years old, and 13 people over the age of 60. There were differences in the gender distribution of infected patient in different age groups (P≤0.001).
Table 1: Number of confirmed cases, asymptomatic patients, and relevant individuals in Putian City, Fujian Province, from Sep- tember 10 to September 25, 2021.
| Date | Confirmed cases |
Asymptomatic patients |
Relevant individuals |
|---|---|---|---|
| 10, Sep | 1 | 4 | 318 |
| 11, Sep | 19 | 17 | 897 |
| 12, Sep | 15 | 13 | 1132 |
| 13, Sep | 24 | 1 | 1102 |
| 14, Sep | 33 | 0 | 1375 |
| 15, Sep | 38 | 0 | 1687 |
| 16, Sep | 28 | 6 | 1004 |
| 17, Sep | 21 | 0 | 878 |
| 18, Sep | 4 | 0 | 321 |
| 19, Sep | 7 | 0 | 584 |
| 20, Sep | 5 | 0 | 764 |
| 21, Sep | 2 | 0 | 253 |
| 22, Sep | 3 | 0 | 377 |
| 23, Sep | 4 | 0 | 310 |
| 24, Sep | 1 | 0 | 199 |
| 25, Sep | 0 | 0 | 0 |
Note: Relevant individuals refer to close contacts, sub-close con- tacts, and space-time accompanying contacts.
The scope of screening was gradually expanded according to the number of the infected found, and the observation sites were timely increased based on the number of relevant individuals tracked by epidemiological investigation, so as to meet the needs of centralized medical observation. As of September 25, 2021, a total of 110 centralized medical observation sites were put into use in Putian city. The information on the distribution of centralized medical observation sites, the using of rooms, isolated relevant individuals and so on in Putian is shown in Table 2.
Table 2:The setting of centralized medical observation places and the situation of people who take centralized medical observation in Putian city.
| Centralized medical observation sites |
Using of rooms |
Isolated relevant individuals |
Underlying diseases |
|
|---|---|---|---|---|
| Xianyou | 21 | 1599 | 2035 | 70 |
| Licheng | 34 | 2984 | 3737 | 89 |
| Chengxiang | 21 | 2300 | 2328 | 85 |
| Hanjiang | 18 | 1259 | 1301 | 84 |
| Xiuyu | 10 | 1051 | 1051 | 27 |
| Meizhou | 0 | 0 | 0 | 0 |
| Beian | 6 | 565 | 749 | 17 |
Note: As of September 25, 2021, Putian city has set up a total of 110 centralized medical observation sites, opened 9758 rooms, and ac- cumulated 11,201 people under centralized observation, of which 372 patients have underlying diseases such as hypertension and diabetes.
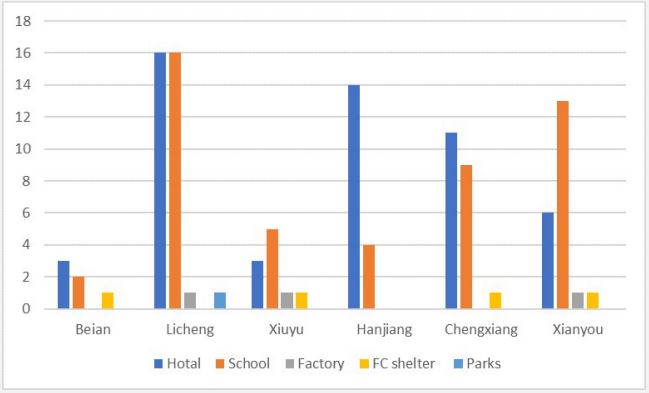
The centralized medical observation sites in Putian city were mainly obtained through the transformation of hotels (53) and schools (49), which account for 92.7% of all centralized medical observation sites. In addition, four makeshift hospitals were temporarily built, and three factory buildings and a park were requisitioned (Figure 3).
In order to ensure the safe and orderly implementation of the centralized medical observation, according to the guidelines of the National Health Commission of China for the prevention and control of the Novel Coronavirus pneumonia epidemic, the management systems and the workflow intended for different posts and work requirements were developed, including personnel management, health monitoring, nucleic acid testing, medical care, referral and transfer, supervision and inspection, material supply, waste disposal, disinfection and cleaning, personal protection, publicity and education and so on; Doctors, Nurses, logistics personnel, volunteers, grid administrators, community cadres and downward dispatched officials, etc. were selected and dispatched to form a special class, with a clear division of labor, detailed responsibilities, and be responsible for the overall management of centralized medical observation. During the epidemic, according to the work needs, a total of 263 doctors, 340 nurses, 1,166 logistics personnel, 228 volunteers, 153 grid administrators, 11 community cadres and 1,012 downward dispatched officials were transferred to various centralized medical observation sites in Putian city to undertake the task of epidemic prevention and control (Table 3).
Table 3: Putian city centralized medical observation sites work staff.
| DOC | NUR | LP | VOL | GA | CC | DDO | |
|---|---|---|---|---|---|---|---|
| Xianyou | 43 | 84 | 165 | 75 | 10 | 1 | 153 |
| Licheng | 97 | 106 | 465 | 75 | 34 | 0 | 228 |
| Chengxiang | 51 | 70 | 220 | 40 | 35 | 2 | 370 |
| Hanjiang | 36 | 32 | 153 | 18 | 74 | 8 | 78 |
| Xiuyu | 21 | 34 | 131 | 18 | 0 | 0 | 59 |
| Meizhou | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Beian | 15 | 14 | 32 | 2 | 0 | 0 | 124 |
Putian city centralized medical observation sites source. Putian city obtained enough centralized medical observation places through the transformation of hotels, schools, factories, etc., of which hotels and schools were the main sources, accounting for 48.18% and 44.55% respectively.
Discussion
It was found that children under the age of 15 account for a large proportion (40.24%) of the infected in this round of epidemic in Putian city, which is slightly different from previous epidemics reported in China [29-31]. This was considered to be possibly related to the outbreak of the epidemic in schools, with closed classroom environments, more collective activities and easy gathering of students, which provides favorable conditions for virus transmission; also, it may be related to vaccination, as of September 2021, no vaccination work of COVID-19 for minors under the age of 15 was carried out in China, and the effective vaccine protection was not provided for this group, and Putian city has completed the full vaccination of people aged 16-60 in September 2021. When we conducted a statistical test on the infection rate of the whole population in Putian City, the two also showed a significant difference (P=0.028). However, the infection of the vaccinated population also confirmed that the mutant virus has the ability to break through the vaccine immune barrier [5,6]. This reminded us to attach great importance to the issues of virus mutation and breakthrough infection, actively track and monitor, and timely adjust the vaccination policy based on extensive evidence to establish the immune barrier for the whole population as soon as possible [5,9,32,33].
Centralized medical observation is an effective way to respond to the COVID-19. Especially when a clustered outbreak occurred in a local area, isolation measures are taken for highrisk groups, with the implementation of centralized medical observation, restrictions on their actions and reduced contacts. This can timely break the chain of virus transmission and realize “zero new cases” of the infected in the community as soon as possible to quickly curb the further spread of the epidemic [20,24,28]. The key to why the epidemic was controlled within a “one incubation period” or so in Putian lied in the early adoption of centralized isolation measures to limit relevant individuals to designated places for medical observation. Therefore, in the late stage of the epidemic, the newly infected in Putian were basically screened through active nucleic acid testing in the centralized medical observation site, which is a real-world evidence for the efficient role of centralized medical observation in the response to the epidemic
During the outbreak of the epidemic, the implementation of large-scale centralized medical observation is not only an emergency disposal task, but also a systematic and comprehensive work, involving various aspects such as site requisition, personnel dispatch, organization and arrangement, work mobilization, material supply, living security. Therefore, It is necessary to have a unified and highly-efficient command and leadership mechanism, as well as the coordinated participation and strong support of multiple departments [34-36]. In response to this epidemic, the Fujian provincial government set up a front-line headquarters for epidemic disposal in Putian city, which immediately launched the level-2 emergency response plan, with frontline leadership, upgraded command and flat management. The peacetime and wartime working modes were quickly converted to activate the command system of the epidemic prevention and control; nine working groups, including comprehensive coordination, nucleic acid sampling and testing, epidemiological investigation, medical treatment, publicity, scientific research and tackling the key research project, foreign affairs, logistics support and public security prevention and control were set up and a cross-departmental cooperation mechanism was established; each working group regularly organized consultation meetings every day to exchange the latest information, solve practical difficulties and problems; the response measures were dynamically adjusted according to the progress of the epidemic, and all security work was coordinated under the leadership of the front-line headquarters to ensure the orderly and stable implementation of centralized medical observation.
The implementation of centralized medical observation requires the provision of sufficient sites in a short time, and it needs to be constantly adjusted with the changes in epidemiological investigations and tracked relevant individuals. It is a specific measure taken by the Chinese government to respond to local epidemic outbreaks, an important means of sacrificing the freedom and rights of a small number of people in exchange for the lives, health and safety of the majority of people, and an important embodiment of the concerted efforts of government departments, social organizations and individuals to protect public health. Also the implementation of centralized medical observation is a major test on the ruling level and governance ability of local governments [37,38]. In the early stage of this round of epidemic outbreak, Putian city also faced difficulties such as insufficient number of centralized medical observation sites, non-standard internal space layout, and inability to optimize and transform the external environment. As a result, there was a lack of management and control for a large number of relevant individuals due to insufficient sites for centralized medical observation, thus resulting in the expansion of transmission. Putian municipal government raised funds in various ways, coordinated and integrated the resources of the whole city. On the basis of requisitioning hotels, Putian municipal government took advantage of the opportunity of school suspension to carry out emergency transformation of student dormitories, opened up a large number of sites for centralized medical observation in a short time, and properly solved the practical difficulties. Of course, this also warned us that even after the epidemic is over, we should make emergency reserves of centralized medical observation sites to respond to possible disease pandemics in the future.
Obviously, it is not only a difficult decision, but a huge challenge to make people strictly abide by the mandatory isolation requirement of single-person and single-room without social visits for 14 consecutive days [39,40]. Therefore Putian city launched a new initiative of “remote observation”, namely, relevant individuals in the same place are disrupted and dispersed to different places for cross-regional centralized medical observation. It can also be seen from the results of this study that in addition to Xianyou County with the most reported cases. Licheng District, Chengxiang District, Hanjiang District, etc. also set up more centralized medical observation sites, because these areas have relatively rich hotel and school resources, which can be quickly transformed into centralized medical observation sites to meet the needs of “remote observation”. This will prevent people from violating regulations in familiar places, and help them strictly abide by the requirements of epidemic prevention and control.
In addition, psychological problems during centralized medical observation are also of very high concern. During the epidemic, especially after compulsory measures are taken, both the isolated relevant individuals and the staff in the centralized medical observation sites can encounter various psychological problems [41-43]. Therefore, a psychological assistance team was set up to carry out itinerant diagnosis and treatment in 110 centralized medical observation sites in the city. The psychological counseling hotline and care platforms were opened to provide 24-h psychological counseling and assistance as well as all-round psychological counseling and humanistic care for relevant individuals and on-site staff. Owing to the adoption of targeted interventions, various psychological problems were effectively alleviated.
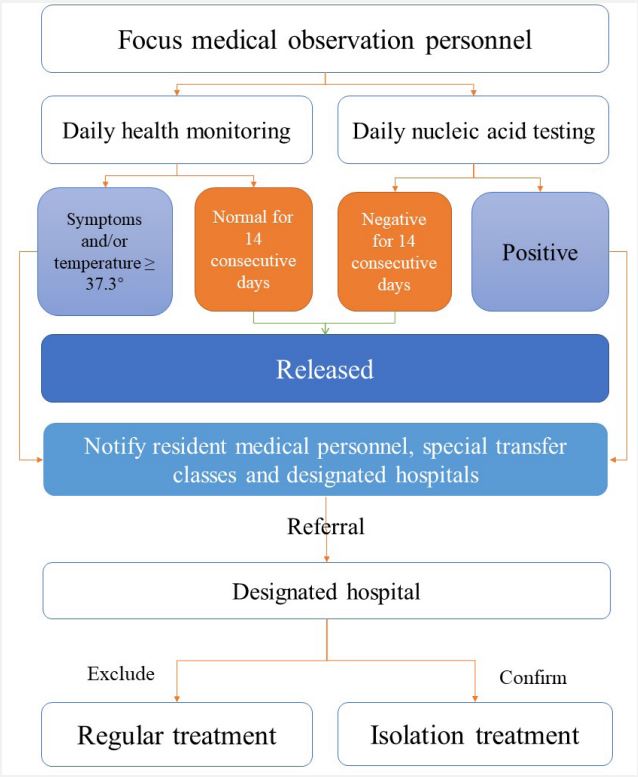
Due to the clustered outbreak of the epidemic in a short time as well as the limitation of time and nucleic acid testing ability, accurate screening was not achieved [44]. In order to curb the spread of the epidemic as quickly as possible, mandatory centralized medical observation was implemented, but this is only a means and Its main purpose is to find those potentially infected as soon as possible during the observation period to cut off the transmission route in time [11,16,22,28]. Therefore, a working mechanism and emergency plan for the monitoring, detection, referral of those potentially infected were established, with the construction of an informatization registration and reporting system. During the 14-day isolation for the centralized medical observation, daily temperature monitoring, health report and nucleic acid testing are required for relevant personnel every day. Once the individuals with suspected clinical symptoms of the novel pneumonia and/or the body temperature (≥37.3°) and a positive nucleic acid test for two consecutive times were found, the emergency plan would be initiated immediately and they would be transferred to the designated hospital for the treatment of the novel conoravirus pneumonia by special personnel and vehicles for review, confirmation and isolation treatment (Figure 4).
Putian city centralized medical observers for medical treatment and referral process. In order to strengthen personnel management, Putian city has formulated a detailed process for centralized medical observers to seek medical treatment and referral, and designated special personnel and special vehicles to be responsible for the transfer work.
As an important measure to respond to the COVID-19, infection prevention and control during the period of centralized medical observation is the top priority, and preventing crossinfection is the key to stopping the further spread of the epidemic [22,28,45]. Thus, during the epidemic response in Putian, innovative technologies such as the Internet were adopted to carry out online training and trained the staff in centralized medical observation sites in infection and control systems and workflows such as wearing and taking off personal protective equipment, environmental disinfection and cleaning, medical waste disposal to enhance their infection prevention and control awareness and management capabilities. The mobile social media platform was used to promote the knowledge of health education as well as epidemic prevention and control, carry out the health education of personal hygiene and self-protection for relevant individuals to improve their self-protection awareness and skills. At the same time, infection prevention and control experts at the national, provincial and municipal levels were selected and transferred to form a special working group to conduct “three fixed” inspections (fixed time, fixed person and fixed point) on the infection prevention and control of 110 centralized medical observation sites in Putian, achieving full coverage, no dead corners and zero infection.
Limitations
First of all, regrettably, due to the lack of sufficient psychological professionals and the requirements of emergency response, it was impossible and not allowed for us to conduct in-depth interview with relevant individuals with psychological problems in centralized medical observation sites and perform detailed investigation on their psychological problems. Therefore, the analysis and research in this regard were carried out and we hope to make a breakthrough in the future; Secondly, Due to the limitations of the research site, our views may have certain defects in representation, such as not taking into account factors such as population, economic development level, and mobilized resources. Finally, what was described in this paper was the emergency measures taken during the secondlevel response stage of public health emergencies. There was no previous research results available for us to compare their effectiveness and roles under different levels of emergency response, but we believe that these practices introduced are reproducible, operable and propagable.
Conclusion
At present, the ever-changing the Novel Coronavirus is still a serious threat to human health and public health safety and it can not be the last biosecurity crisis we face. In the cruel reality, it has been proved that no one is immune to the virus, and as mentioned in the series of articles on “China`s response to covid-19” in the BMJ “no one is safe until everyone is safe”. What is different from the other existing research is that in this study Chinese practices and experience of centralized medical observation was introduced in the face of local outbreaks of the novel coronavirus epidemic during the “dynamic zero” stage of precise epidemic prevention and control, which is beneficial to the consolidation and expansion of the achievements of the epidemic prevention and control strategy and deepen the understanding of this strategy.
We know that the role of any single measure in the face of the COVID-19 is limited, and the response methods are also different in each country. However, our practice and research have showed that in addition to the isolation function, centralized medical observation also undertakes the tasks such as health monitoring, nucleic acid testing, medical services, living security, psychological assistance, infection prevention and control for those potentially infected, and it is an effective and practical strategy to respond to the epidemic of major and severe infectious diseases transmitted by air or direct contact such as the COVID-19. It is a more valuable and responsible means of prevention and control for human health. Our experience in this regard can provide some reference for the other countries to help the whole world end the epidemic and restore nomal life as soon as possible and also prepare for the possible pandemic of other unknown infectious diseases in the future.
Declarations
Definition
Close contacts: Refers to the individuals who had close contact with them but took no effective protection two days before the appearance of the symptoms of suspected cases and confirmed cases, or 2 days before the sampling of asymptomatic patients.
Sub-close contacts: Refers to the individuals who had close contact with the close contact such as living together, working in the same closed environment, dining together and having entertainment but took no effective protection measures from the first contact (refers to the first contact between the close contact and confirmed cases or asymptomatic patients from 2 days before the onset of the confirmed cases or 2 days before the sampling of the asymptomatic patients until the isolation management and control) between a close contact and confirmed cases or asymptomatic patients until the close contact was managed in isolation.
Space-time accompanying contacts: Refers to the mobile phone number owners who stayed in the same space-time grid (800 m * 800 m) with the mobile phone numbers of confirmed cases and asymptomatic patients for more than 10 minutes and also the cumulative stay time in the last 14 days exceeded 30 h.
Ethics approval: The need for approval was waived by the local ethical committees as data were reported anonymously, and all participants agreed to the study. During the data collection period, Putian city was in the secondary response stage of public health emergencies, and the written informed consent was waived, which belongs to the emergency management of public health incidents.
Consent for publication: Not applicable.
Availability of data and materials: Part of the data for this study is publicly available and can be obtained from the official website of the local government. Part of the data is not public, but can be obtained from the corresponding author if required for research.
Competing interests: None declared.
Funding: This study was supported by grants from the Scientific and Technological Innovation Joint Capital Projects of Fujian Province (No.2022R0088), and the Fujian Provincial Medical and Health System Reform Research Association Health Policy Innovation Research Project (No.2022B07), China.
Acknowledgements: Not applicable.
Authors’ contributors: JJ obtained funding and designed the study. JJ, XJH, and STW collected the data. JJ, WQR and XWT were involved in data cleaning and analyzed. All authors have read and approved the final manuscript.
References
- Thirty-two ministers of health. The world must act now to be prepared for future health emergencies. BMJ. 2021; 375: n2879.
- Dhama K, Khan S, Tiwari R, et al. Coronavirus Disease 2019-COVID-19. Clin Microbiol Rev. 2020; 33(4): e00028-20.
- Clark H, Sirleaf EJ. Ending this pandemic and securing the future. BMJ. 2021; 375: n2914.
- Vaidyanathan G. Coronavirus variants are spreading in India - what scientists know so far. Nature. 2021; 593(7859): 321-322.
- Khan WH, Hashmi Z, Goel A, et al. COVID-19 Pandemic and Vaccines Update on Challenges and Resolutions. Front Cell Infect Microbiol. 2021; 11: 690621.
- Callaway E. Beyond Omicron: what is next for COVID’s viral evolution. Nature. 2021; 600(7888): 204-207.
- Tu H, Hu K, Zhang M, et al. Effectiveness of 14 day quarantine strategy: Chinese experience of prevention and control. BMJ. 2021; 375: e066121.
- Huang J, Liu X, Zhang L, et al. The oscillation-outbreaks characteristic of the COVID-19 pandemic. Natl Sci Rev. 2021; 8(8): nwab100.
- Ahn DG, Shin HJ, Kim MH, et al. Current Status of Epidemiology, Diagnosis, Therapeutics, and Vaccines for Novel Coronavirus Disease 2019 (COVID-19). J Microbiol Biotechnol. 2020; 30(3): 313-324.
- Zhang Y, Quigley A, Wang Q, et al. Non-pharmaceutical interventions during the roll out of covid-19 vaccines. BMJ. 2021; 375: n2314.
- Wu S, Neill R, De Foo C, et al. Aggressive containment, suppression, and mitigation of covid-19: Lessons learnt from eight countries. BMJ. ; 375: e067508.
- Wen J, Su Z. Public health lessons from crisis-related travel: The COVID-19 pandemic. J Infect Public Health. 2021; 14(1): 158-159.
- Perotte R, Sugalski G, Underwood JP, et al. Characterizing COVID-19: A chief complaint based approach. Am J Emerg Med. 2021; 45: 398-403.
- Haghighi-Morad M, Alavi Darazam I, Bahrami-Moltagh H, et al. Atypical presentation of COVID-19; an observational retrospective study. BMC Infect Dis. 2020; 20(1): 870.
- Gao W, Lv J, Pang Y, et al. Role of asymptomatic and pre-symptomatic infections in covid-19 pandemic. BMJ. 2021; 375: n2342.
- Mackenzie JS, Smith DW. COVID-19-A Novel Zoonotic Disease: A Review of the Disease, the Virus, and Public Health Measures. Asia Pac J Public Health. 2020; 32(4): 145-153.
- Chen Q, Rodewald L, Lai S, et al. Rapid and sustained containment of covid-19 is achievable and worthwhile: implications for pandemic response. BMJ. 2021; 375: e066169.
- Rudan I. Answering the initial 20 questions on COVID-19 (January-February 2020). J Glob Health. 2020; 10(1): 010106.
- Chen S, Zhang Z, Yang J, et al. Fangcang shelter hospitals: A novel concept for responding to public health emergencies. Lancet. 2020; 395(10232): 1305-1314.
- Du B, Wang C, Singer M. Learning for the next pandemic: The Wuhan experience of managing critically ill people. BMJ. 2021; 375: e066090.
- Ayouni I, Maatoug J, Dhouib W, et al. Effective public health measures to mitigate the spread of COVID-19: A systematic review. BMC Public Health. 2021; 21(1): 1015.
- Haldane V, Jung AS, De Foo C, et al. Strengthening the basics: Public health responses to prevent the next pandemic. BMJ. 2021; 375: e067510.
- Zhou Y, Jiang H, Wang Q, et al. Use of contact tracing, isolation, and mass testing to control transmission of covid-19 in China. BMJ. 2021; 375: n2330.
- Ehmann MR, Zink EK, Levin AB, et al. Operational Recommendations for Scarce Resource Allocation in a Public Health Crisis. Chest. 2021; 159(3): 1076-1083.
- Czeisler MÉ, Howard ME, Robbins R, et al. Early public adherence with and support for stay-at-home COVID-19 mitigation strategies despite adverse life impact: A transnational crosssectional survey study in the United States and Australia. BMC Public Health. 2021; 21(1): 503.
- Humeyestewa D, Burke RM, Kaur H, et al. COVID-19 response by the Hopi Tribe: impact of systems improvement during the first wave on the second wave of the pandemic. BMJ Glob Health. 2021; 6(5): e005150.
- Zou X, Song LX, He JF, Lu JH, Wang JZ. Analysis of 2063 COVID-19 close contacts by centralized medical observation in Shenzhen City. Chin J of PHM. 2021; 37(4): 557-559.
- Wang W, Huang C, Pang XH, et al. Performance of COVID-19 centralized isolation medical observation points in Beijing. Chin J Public Health.2021; 37(7): 1077-1081.
- Mei X, Zhang Y, Zhu H, et al. Observations about symptomatic and asymptomatic infections of 494 patients with COVID-19 in Shanghai, China. Am J Infect Control. 2020; 48(9): 1045-1050.
- Tian S, Hu N, Lou J, et al. Characteristics of COVID-19 infection in Beijing. J Infect. 2020; 80(4): 401-406.
- Qiu H, Wu J, Hong L, et al. Clinical and epidemiological features of 36 children with coronavirus disease 2019 (COVID-19) in Zhejiang, China: an observational cohort study. Lancet Infect Dis. 2020; 20(6): 689-696.
- Wang J, Jing R, Lai X, et al. Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines (Basel). 2020; 8(3): 482.
- An Z, Wang F, Pan A, et al. Vaccination strategy and challenges for consolidating successful containment of covid-19 with population immunity in China. BMJ. 2021; 375: e066125.
- Jung AS, Haldane V, Neill R, et al. From dichotomisation towards intersectionality in addressing covid-19. BMJ. 2021; 375: e067500.
- Kitchanapaibul S, Udplong A, Apidechkul T, et al. Experiences and expectations regarding COVID-19 prevention and control measures among the hill tribe population of northern Thailand: a qualitative study. BMC Public Health. 2021; 21(1): 1060.
- Singh S, Bartos M, Abdalla S, et al. Resetting international systems for pandemic preparedness and response. BMJ. 2021; 375: e067518.
- Shen J, Duan H, Zhang B, et al. Prevention and control of COVID-19 in public transportation: Experience from China. Environ Pollut. 2020; 266(Pt 2): 115291.
- Donnelly A. Creating a new global treaty to minimise future pandemic risks. BMJ. 2021; 375: n2784.
- Hassan SM, Ring A, Tahir N, et al. The impact of COVID-19 social distancing and isolation recommendations for Muslim communities in North West England. BMC Public Health. 2021; 21(1): 812.
- Hua J, Shaw R. Corona Virus (COVID-19) Infodemic and Emerging Issues through a Data Lens: The Case of China. Int J Environ Res Public Health. 2020; 17(7): 2309.
- Qiu J, Shen B, Zhao M, et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen Psychiatr. 2020; 33(2): e100213.Copyright © 2024 Jiang J. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Su ZH, McDonnell D, Wen J, et al. Mental health consequences of COVID-19 media coverage: The need for effective crisis communication practices. Global Health. 2021; 17(1): 4.
- Thielsch MT, Röseler S, Kirsch J, et al. Managing pandemics Demands, resources, and effective behaviors within crisis management teams. Appl Psychol. 2020. 10.1111/apps.12303.
- Russell TW, Wu JT, Clifford S, et al. Effect of internationally imported cases on internal spread of COVID-19: A mathematical modelling study. Lancet Public Health. 2021; 6(1): e12-e20.
- Tang JL, Abbasi K. What can the world learn from China’s response to covid-19? BMJ. 2021; 375: n2806