Research Article
Volume 3, Issue 6
Predictive Value of Six-Minute Walking Test in Post-Acute Myocardial Infarction Patients in Benghazi
Essam A Eldenna1 ; Faiza A Elhamdy2 ; Nagwa Elghryani3,4*; Mohamed M Khamis
1Faculty of Medicine, Department of Community Medicine, University of Benghazi, Benghazi, Libya.
2Faculty of Medicine, Department of Physiology, University of Benghazi, Benghazi, Libya.
3School of Veterinary Medicine, University College Dublin, D04 W6F6 Dublin, Ireland.
4Department of Biology, University of Benghazi, Benghazi 1308, Libya.
Corresponding Author :
Nagwa Elghryani
Tel: +35-31368027;
Email: Libya.najwa75@gmail.com
Received : Apr 30, 2024 Accepted : May 27, 2024 Published : Jun 03, 2024 Archived : www.meddiscoveries.org
Citation: Eldenna EA, Elhamdy FA, Elghryani N, Khamis MM. Predictive Value of Six-Minute Walking Test in Post-Acute Myocardial Infarction Patients in Benghazi. Med Discoveries. 2024; 3(6): 1162.
Copyright: © 2024 Elghryani N. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background: Acute Myocardial Infarction (AMI) poses a significant threat to heart health. The six-Minute Walking Test (6MWT) assesses patients’ ability to walk the longest distance possible on a level course in six minutes, with parameters like arterial pressure, heart rate, and oxygen saturation monitored.
Aim: We sought to determine whether the 6MWT predicted cardiovascular events post myocardial infarction patients. This study investigates the predictive value of the Six-Minute Walking Test (6MWT) in post-AMI patients, assessing their ability to perform daily activities and evaluating the effectiveness of medical therapy and rehabilitation programs.
Methods: This was an interventional study in a cohort of 71 patients (aged 18-75) who were admitted to the cardiac care unit at Alhawary Cardiac Center and Benghazi Medical Center with a diagnosis of uncomplicated acute MI from March to September 2022. The 6-MWT was administered at two time points: within the first week and after three months post-AMI. The primary outcome was the difference between the mean distance walked between the time points.
Results: The study findings demonstrated a marked enhancement in average walking distance, accompanied by a reduction in complications, particularly among patients engaged in rehabilitation programs. The 6MWT was well tolerated among all participants. The mean distance covered during the initial assessment (404±35.8 meters) was significantly increased during the subsequent evaluation (546±37.1 meters) (p<0.0001). Patients who adhered to a rehabilitation program exhibited a significant increase in distance walked (146±15 meters) (p<0.005), and showed a decrease in BMI. Furthermore, improvements of heart rate and grade of dyspnea (from grade II to grade I) were observed during the second assessment compared to the first.
Conclusion: Our results indicate that 6MWT holds predictive value for post-AMI mortality and morbidity rates. These findings offer valuable insights for patient care and serve as a foundation for healthcare reform efforts.
Keywords: 6MWT; Acute myocardial infarction; Exercise test; Post-MI complications.
Introduction
Cardiovascular health is influenced by various conditions, including arrhythmia, high blood pressure, coronary heart disease, valvular heart disease, and Myocardial Infarction (MI) [1]. MI, characterized by heart discomfort and pain in the arm on the side of the heart, represents a common cause of heart failure, affecting approximately 1.3 million individuals annually [2,3], and its presentation changes significantly with age [4]. Its severity depends on factors such as the number and location of blocked vessels [5].
Prompt diagnosis and treatment are paramount in managing Myocardial Infarction (MI), given its association with over 200 risk factors [6-9]. These risk factors encompass various demographic and lifestyle aspects such as old age, male gender, black race, family history, elevated lipid levels, hypertension, diabetes, obesity, alcohol consumption, smoking, sedentary lifestyle, and stress. Current therapeutic modalities include thrombolysis and Percutaneous Coronary Intervention (PCI) [10,11]. Failure to promptly and appropriately manage acute MI can significantly escalate the risk of mortality and further cardiovascular complications. Early engagement in rehabilitation programs following discharge is crucial to mitigate complications and expedite recovery [12,13].
Exercise tests, notably stress tests and the Six-Minute Walking Test (6MWT), hold significant utility in evaluating the functional capacity of post-MI patients. Originally devised for chronic respiratory diseases, the 6MWT has garnered attention in cardiology due to its simplicity and efficacy. Unlike more elaborate assessments, it does not necessitate expensive equipment or specialized technician training.
Conducted along a 30 meter corridor, the 6MWT evaluates a patient’s ability to cover the longest distance possible in six minutes, while monitoring parameters such as arterial pressure, heart rate, and oxygen saturation. Its versatility extends beyond mere assessment to include predicting improvements in exercise capacity and aiding in the selection of appropriate cardiac rehabilitation strategies [14].
The utilization of the 6-Minute Walk Test (6MWT) in assessing cardiovascular health emerged just over 15 years ago [15], marking a significant advancement in diagnostic methodologies for heart disease. Since its inception, extensive research has elucidated its efficacy in measuring functional limitation, evaluating therapy effects, and stratifying prognosis in chronic heart failure and myocardial infarction. Notably, impairment of exercise capacity post-infarction has emerged as a crucial prognostic indicator, emphasizing the pivotal role of the 6MWT in diagnostic and prognostic paradigms. One of the notable attributes of the 6MWT is its provision of a safe and practical means to evaluate patients’ functional capacity, demonstrating correlation with submaximal treadmill exercise. Furthermore, patient preference for the 6MWT over conventional exercise tests is attributed to its similarity to activities of daily living [16], enhancing its clinical relevance and patient compliance.
The outcomes of the 6MWT are influenced by numerous determinants, encompassing factors beyond cardiovascular parameters such as muscular strength, postural balance, reaction time, mood, and general health. Additionally, anthropometric variables including age, gender, and weight impact test results, underlining the necessity of establishing normative values and reference equations for result interpretation.
Given the global prevalence of Coronary Heart Disease (CHD), effective prevention and management strategies are imperative. In this context, the assessment of physical functional capacity assumes significant importance, closely associated with CHD prognosis. While maximal exercise testing offers detailed insights, the 6MWT presents a practical and accessible submaximal alternative, instrumental in evaluating functional capacity, responsiveness to therapy, and predicting morbidity and mortality in heart disease patients. Nonetheless, understanding its strengths and limitations compared to maximal exercise testing is crucial for its appropriate application in clinical settings.
Despite its designation as a submaximal test with a maximum duration of 6 minutes, the 6MWT presents characteristics that challenge its classification. Studies indicate a medium to high correlation between the longest distance walked during the test and peak oxygen uptake measured during maximal exercise tests, underscoring its potential for prognostic significance and reproducibility in predicting mortality and morbidity in heart failure patients.
In this study, our objective is to assess the predictive value of the 6MWT in Post-Acute Myocardial Infarction (AMI) patients in Benghazi, Libya-a region characterized by historically high rates of chronic diseases. Through participant interviews, examinations, laboratory investigations, Electrocardiography (ECG), and echocardiography studies, we aim to elucidate patients’ daily activity performance, evaluate the efficacy of post-MI management strategies, and analyze mortality and morbidity rates. By presenting comprehensive data analyses, we endeavor to provide healthcare practitioners with valuable insights to guide the reduction of post-MI complications and optimize patient care.
Material and methods
Subjects
This cross-sectional interventional study employed a random sample of 71 subjects admitted or discharged from the Cardiac Care Unit (CCU) at Alhawary Cardiac Center and Benghazi Medical Center within 24 hours of an uncomplicated Acute Myocardial Infarction (AMI) diagnosis. The study period extended from March 2022 to September 2022, encompassing both ST-Segment Elevation Myocardial Infarction (STEMI) and non-STEMI cases, irrespective of reperfusion therapy (conservative, thrombolysis, or percutaneous coronary intervention).
The inclusion criteria for participant selection in this study are individuals who have experienced a confirmed Myocardial Infarction (MI), verified through acute elevation of cardiac enzymes and specific Electrocardiogram (ECG) changes, specifically ST-segment elevation. The eligible age range for inclusion is between 18 and 75 years, and participants should be in stable clinical and hemodynamic conditions.
Excluded are individuals with recurrent or refractory pain, those presenting neuromuscular disorders, patients with persistent arrhythmias, and those with prior conditions associated with exercise intolerance. Participants showing signs or symptoms of angina or chest discomfort at rest, experiencing unstable blood pressure levels, exhibiting signs of active infection, or raising ethical concerns are also excluded from the study. These criteria are established to ensure a specific and controlled participant group for the research study.
Patient preparation
Official consent was obtained from the administrations of Benghazi Medical Center and Benghazi Cardiac Center, as well as from individual patients. Patients were briefed on the study’s objectives, benefits, and potential risks, ensuring anonymity. Language barriers and educational challenges were taken into account.
A comprehensive medical history, clinical examination, imaging, and laboratory tests were conducted, with weight and height measurements recorded. Patients adhered to diet and exercise plans as per physician recommendations. Detailed instructions regarding the 6-Minute Walk Test (6MWT) were provided to all patients prior to testing. All investigations and testing were carried out under the supervision of expert staff. Participants were advised to wear comfortable clothing and appropriate footwear, with ordinary walking aids permitted. Before the test, patients were instructed to refrain from exertion for 2 hours and were allowed to consume a light meal.
6MWT protocol
The 6MWT was conducted in two sessions: the first during the first week following myocardial infarction, and the second three months later.
Participants walked between two cones set 30 meters apart, with their walking distance measured over 6 minutes. Dyspnea levels were assessed using the Rating of Perceived Exertion (RPE) scale. Blood pressure, heart rate, and oxygen saturation were monitored before, during, and after the test. ECG testing (Hi-Tech model 2015 USA) was performed after completion of the 6MWT or if necessitated by the onset of chest pain. Patients were permitted to take breaks or lean against a wall as needed, and an oxygen tank was available upon request.
Standardized verbal encouragement was provided at specific intervals to motivate participants, and continuous monitoring ensured participant safety throughout the procedure.
Statistical analysis
Results were presented as mean ± standard deviation for continuous variables or as number/percentage for categorical variables. Group comparisons were conducted using unpaired Student’s t-tests for continuous variables and Chi-square tests for categorical data.
All statistical analyses were performed using statistical software (SPSS version 23, IBM). A p-value<0.05 was considered statistically significant.
Results
Descriptive statistics of the sample
The study included a total of 71 subjects with an age range of 18-74 years and a mean age of 53.4±10 years. The highest proportion of participants fell within the age group of 50-69 years (28.2%), while the lowest age group was >70 years (7%) (Table 1). Approximately 60% of the sample were male (Table 1), and a predominant majority, 86%, were White (Table 1).
In the first test, 15.5% of participants had a normal Body Mass Index (BMI), 25.4% were overweight, and 19.6% and 31% were classified under grade I and grade II obesity, respectively. About 76% of the sample were categorized as high-risk patients. The mean BMI in the first test was 35.9 kg/m2 ; SD±7.6. In the second test, 21.9% had a normal BMI, 30.9% were overweight, and 14% and 21.4% were classified under grade I and grade II obesity, respectively. The percentage of high-risk patients decreased to 34.1%. The mean BMI in the second test was 30.3; SD± 6.9 (Table 2).
Classification of the sample according to chronic diseases and complications post-MI
In both the first and second tests, over 66.3% of the sample had chronic diseases, with diabetes recorded in 11.3%, hypertension in 22.5%, and both diabetes and hypertension in 15.5% (Table 3). In the second test, more than 25% of the sample experienced complications post-discharge from the hospital following myocardial infarction. The majority (83.33%) of complications were attributed to heart failure, while 16.6% experienced another infarction.
Baseline characteristics according to modality of treatment in acute MI and post-MI rehabilitation programs
The management of acute MI in the Critical Care Unit (CCU) involved standard protocols, with 100% of patients receiving coronary perfusion therapy, antiplatelets/aspirin, Angiotensin Channel Blocker (ACE-I) or Angiotensin Ii Receptor Blockers (ARBs), beta-blockers, and statins. Approximately 15.5% of the sample also received coronary vasodilation nitrates in the first test. In the second test, over 90% of cases continued the same treatment post-discharge from the CCU, and no statistically significant differences were observed.
Baseline characteristics according to the time of first and second tests and measurements during the test
The first test was conducted between the fourth- and seventh-days post-MI, with the majority (56.4%) undergoing the test on the fourth and fifth days, with a mean of 5.4 days; SD±1.1. The second test occurred three months after the first test. Measurements during the test, including Systolic Blood Pressure (SBP), Diastolic Blood Pressure (DBP), Heart Rate (HR), and Oxygen Saturation (SPO2 ), showed no significant changes between the start and end of both tests. However, there was a significant improvement in SPO2 from 97.1±1.5 in the first test to 98.4±0.69 in the second test (p=0.000) (Table 4).
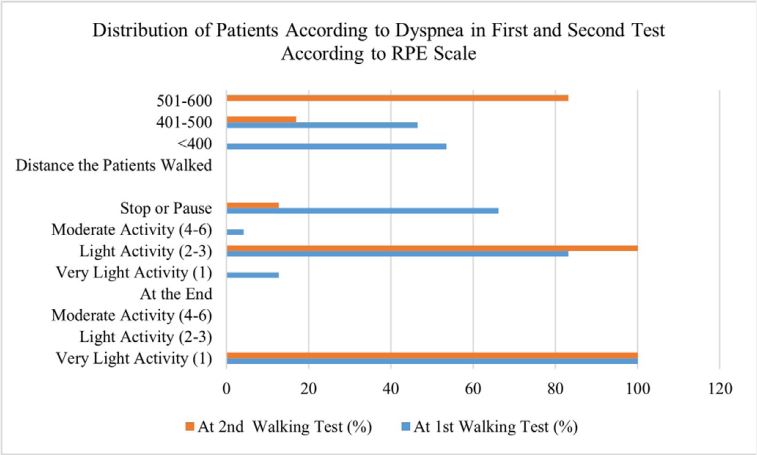
Comparison between the total distance in first and second test
Table illustrates the changes in the distance walked between the first and second tests. In the first test, all patients (100%) walked below 500 meters, with 53.5% walking below 400 meters. In the second test, all patients walked more than 400 meters, with 83.1% covering a distance of 501-600 meters (p<0.0001). At forst walking test: Mean = 404.9; SD±35.8 meters. Minimum = 320 meters. Maximum = 495 meters. Whereas at second walking test: Mean = 546; SD±37.1 meters.
Table 1: Distribution of patients according to age, gender, and (N=71).
| Age/years | % |
|---|---|
| 30-39 | 12.7 |
| 40-49 | 25.4 |
| 50-59 | 28.2 |
| 60-69 | 26.8 |
| ≥70 | 7 |
| Gender | |
| Male | 60 |
| Female | 40 |
| Race | |
| Non-white | 14 |
| White | 86 |
Table 2: Distribution of patients according to BMI 1st test (N=71).
| BMI kg/m2 | 1st Test % | 2nd Test % |
|---|---|---|
| <18.5 (underweight) | 8.5 | 12.6 |
| 25-29.99 (normal wt.) | 15.5 | 21.1 |
| 30-34.99 (over wt.) | 25.4 | 30.9 |
| 35-39.99 (class I obesity) | 19.6 | 14 |
| ≥40 (class II obesity) | 31 | 21.1 |
Table 3: Distribution of patients according to etiology of MI and time since attack at first walking test (N=71).
| Medical History | % |
|---|---|
| No | 36.7 |
| Diabetes | 11.3 |
| Hypertension | 22.5 |
| Diabetes and Hypertension | 15.5 |
| Ischemic Heart Disease | 4.2 |
| Renal Problems | 4.2 |
| Ischemic Heart Disease and Diabetes | 4.2 |
| Ischemic Heart Disease and Hypertension | 1.4 |
| Time since attack at first walking test | |
| Fourth | 29.6 |
| Fifth | 26.8 |
| Sixth | 22.5 |
| Seventh | 21.1 |
Mean: 5.4 SD±1.1 days; Median: 5 days; Minimum: 4 days, Maximam: 7 days 100%
Table 4: Measurements in first and second test (N=71).
| Measurements | At 1st Walking Test | At 2nd Walking Test | P Value |
|---|---|---|---|
| SBP at Start | 131.5±12.9 | 128.2±8.3 | 0.072 (NS) |
| DBP at Start | 85.7±8.5 | 83.9±8.2 | 0.201 (NS) |
| SBP at End | 139.9±10.9 | 139.2±8.4 | 0.669 (NS) |
| DBP at End | 92±9.3 | 89.3±6.9 | 0.051 (S) |
| HR at Start | 83.4±11 | 81.2±9.5 | 0.204 (NS) |
| HR at End | 97.3±13.2 | 98.5±6.9 | 0.498 (NS) |
| Start SPO2 (%) | 97.1±1.5 | 98.4±0.69 | 0.000 (HS) |
Discussion
Study subjects and 6MWT timing
Our study comprised 71 patients with Acute Myocardial Infarction (AMI), averaging 53.4±10.7 years. Notably, 55% fell in the 50-69 age group, indicating a shift towards younger individuals experiencing AMI. Male prevalence was 60.6%, aligning with other studies. The racial distribution reflected 86% White and 14% Black, resembling national statistics. For example, the National Center for Health Statistics found that the incidence of MI is 30% more common in the white population. These results are consistent with the findings of our study. Our study implies a change in AMI demographics, possibly linked to evolving risk factors [17].
The test timings demonstrated variations, with 56.4% in the 4th-5th days of the first test and over 90% after 3 months for the second. Comparisons with other studies reveal divergent protocols, stressing the need for standardized guidelines. In one study, patients were tested on their ability to walk on the third day of their attack [18]. The second test was conducted between 8 to 60 weeks later and the results showed a change in the distance that patients were able to walk, which may have been influenced by their prior experience [18]. In another study, the six-minute walk test was used to assess the quality of life in patients who had undergone coronary artery bypass grafting surgery. The test conducted before the surgery was found to be associated with the patients’ quality of life two months after the surgery [18]. Overall, the quality of life improved in all patients, with greater improvement observed in those who were able to walk more than 350 meters before the surgery (142). Thus, the 6MWT, when employed at different intervals, showcased varied outcomes, suggesting its adaptability in assessing recovery and functional capacity.
The 6-Minute Walking Distance (6MWD)
The 6MWD showed significant improvement between the first and second tests, reflecting positive responses to management. This reinforces the 6MWT’s value in gauging functional improvement and predicting future outcomes.
In our study, we observed the total distance walked by patients during the first test. We found that approximately 53.5% of patients walked less than 400 meters in the first test, while in the second test, nobody walked less than 400 meters. During the first test, 46.5% of patients covered a distance between 401 and 500 meters, whereas only 16.9% covered the same distance in the second test. Moreover, none of the patients walked more than 500 meters in the first test, compared to 83.1% who covered a distance greater than 500 meters in the second test.
The mean distance covered by patients during the first test was 404±35.8 meters, and in the second test, it was 546±37.1 meters. This difference was statistically significant (p-value was 0.0001). In another study, the mean 6-minute walk distance was found to be 400.2±107.8 (137), whereas in another research, the mean walking test was 277.96 (±42.17) (139). According to earlier research, the mean walking test during the first test was 521±64 and 539±70 during the second test (134) [19].
The improvement in the distance covered between the first and second tests indicates a positive response to management and sheds light on the future of such cases.
Risk factors and complications post MI
Herein, we also explore BMI and its correlation with AMI risk. A notable shift in BMI percentages between the two tests, as well as improved walking distance with reduced BMI, stresses the impact of weight loss on functional improvement post-MI. By the second time point, class I obesity decreased from 31% to 14%, class II obesity dropped from 25.4% to 21%, and the percentage of risk factors reduced 66%. Our study demonstrated that, as weight is lost, walking distance improves. This is in line with existing literature, as numerous studies assert the importance of weight management in improving functional capacity. In one study, 251 subjects completed the test at baseline with a BMI of 40.6 kg/m and approximately 129 subjects repeated the test after intervention with a BMI of 35.6kg/m2 and a SixMinute Walking Distance (6MWD) of 535 [480-580] meter at baseline and 599 [522-640] meter at follow up [20]. In another study, the 6MWT provided useful information and an excellent evaluation of the functional capacity of very obese people who underwent bariatric surgery, demonstrating that weight loss after bariatric surgery can result in a real improvement in functional capacity [20].
Prevalence of diabetes, hypertension, and complications post-MI was observed, showcasing a substantial burden of comorbidities. Diabetes was recorded in 11.3%, hypertension in 22.5%, both diabetes and hypertension in 15.5%, ischemic heart disease in 4.2%, renal problems and ischemic heart disease and diabetes in 4.2% each, 1.4% had ischemic heart disease and hypertension, and 36.7% were disease-free. In a similar study, diabetes was detected in 23% of patients and systemic hypertension was detected in 38% of them. In our study, more than 25.4% of patients had complications after an acute MI and were readmitted to the hospital. There were no deaths, and the most prevalent consequences were heart failure (83.3%), followed by re-infarction (16.6%). In another cross-sectional study, heart failure was reduced to 3%, while reinfection reduced to 2% [21].
However, compared to other studies in developed countries, our patients exhibit a higher risk of developing complications due to factors such as bad habits, low education levels, delayed management of acute myocardial infarction, and poor patient monitoring. Additionally, there is no program in place to assess the patient’s risk factors or to provide post-discharge evaluation. Indeed, post-discharge risk assessment programs are warranted in these patient populations.
Complications post-MI were associated with poor prognosis, emphasizing the need for effective management strategies. The low complication rate during the 6MWT suggests its safety and potential as a predictive tool. Thus, our study corroborates the large body of evidence that promotes the 6MWT as a robust modality for functional performance and prognostic value in cardiac and thoracic patients.
Protocols of MI management
Our findings are closely related to MI management protocols, revealing a high adherence to medications like aspirin, beta-blockers, and ACE-I/ARB among MI patients. Our data showed that all patients in the care unit used aspirin or antiplatelet in the first walking test, and 94.4% in the second walking test. However, the difference was not statistically significant (p=0.223). Beta-blockers (cardio-selective) were used by 100% of participants in the first walking test and 93% in the second walking test, and the difference was not statistically significant (p=0.112). Similarly, ACE-I/ARB was used by 100% of patients in the first test and 94.4% in the second test, and the difference was not statistically significant (p=0.223). This was found to be the case with nitrates and dyslipidemia drugs. Likewise, another study found that the differences between the use of aspirin, beta-blockers, and ACE-I/ARB in the first and second walk test groups was also not statistically significant [22].
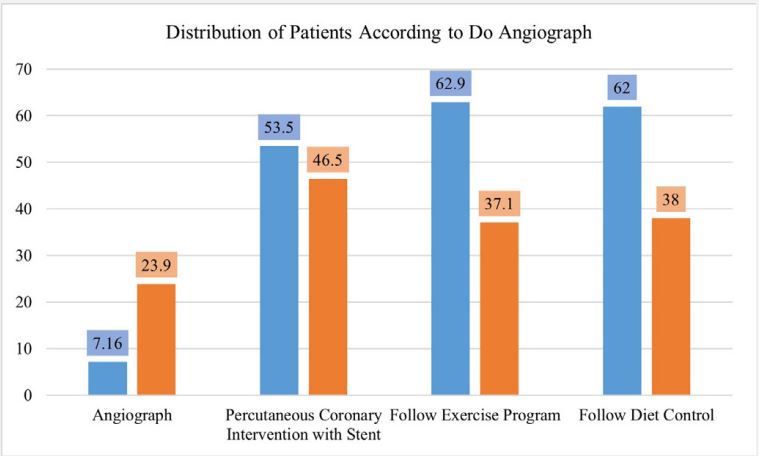
Our study emphasizes the importance of timely intervention, particularly PCI, in improving outcomes. Over 76% of patients underwent coronary angiography, and approximately 53.5% underwent Percutaneous Coronary Intervention (PCI) with a stent to reduce the percentage of problems. PCI should be performed within 90 minutes after first medical contact for ST-Elevation Myocardial Infarction (STEMI), and total ischemia time should not exceed 120 minutes. The walking distance has been shown to increase in patients who underwent early PCI [22]. Our data reflect that, although the same medical protocol was applied in our centers during the acute attack of MI, interventional therapy was not provided or was delayed due to a lack of facilitation.
Effects on vital signs
Evaluation of vital signs during the 6MWT indicated notable correlations. The study recognized improvements in vital signs, supporting the 6MWT’s utility in assessing patients’ acute states and responses to therapy.
During the first walking test, the mean Systolic Blood Pressure (SBP) of patients was 131.5±12.9 mmHg, and the difference was not statistically significant. Another study found that the SBP was 130±21 mmHg in the first walking test and 127±23 mmHg in the second test. The diastolic blood pressure (DBP) was 85.7±8.5 mmHg in the first walking test and 83.9±8.2 mmHg in the second test, and the difference was not statistically significant. In another study, the DBP was 78±11 mmHg in the first walking test and 75±12 mmHg in the second test. There was only a statistically significant difference between the mean levels of the first and second measurement in DBP at the end of the test and at the start.
At the start of the first walking test, the Heart Rate (HR) was 83.4±11 bpm, and in the second walking test, it was 81.2±9.5 bpm, and the difference was not statistically significant. In another study, the HR was 96±12 bpm in the first walking test and 97±14 bpm in the second test.
The oxygen saturation remained constant throughout all the tests, and no participants used an O2 supply. Breathlessness was measured and graded using the Borgs scale. At the start of the first and second walking tests, participants had very light breathing difficulty. At the end of the first test, 12.7% had very little exercise, 83.1% had light activity, and 4.2% had moderate activity. In the second walking test, all participants experienced breathlessness with light exercise. In another study, all patients had very light breathlessness at the start of the first walking test and no breathlessness at all at the completion of the first walking test. At the end of the second walking test, around 90% had very light activity.
Our results are comparable to those of other research, and there was a correlation between the change in vital signs throughout the test and the difference or improvement in vital signs between the first and second tests. This was due to the patients’ acute state and response to therapy.
Importance of rehabilitation programs
Patients following rehabilitation programs demonstrated positive outcomes, linking adherence to diet and exercise with improved 6MWD. Recommendations include integrating 6MWT into post-MI care procedures and conducting follow-up tests for a comprehensive assessment.
Around 62.9% of patients successfully completed their rehabilitation program. They followed a healthy diet and did moderate exercise for half an hour every other day. These individuals did not face any issues after their AMI, and their walking distance improved (6MWD) in the second test. Also, their echocardiography results were better compared to patients who didn’t participate in a rehabilitation program. Several other studies have shown a positive correlation between post-MI therapy and improved outcomes, including increased walking distance [23-28].
Limitations of this study include a small sample size, necessitating larger multi-center studies to support our conclusions. There was a loss of follow-up data in 34 participants due to scheduling and contact difficulties. Lack of patient awareness about the severity of their condition and the importance of rehabilitation limits capturing crucial follow-up data. This, in turn, underscores the need for improved research methodologies in Benghazi clinical settings and patient education initiatives.
Conclusion
Our study presents a comprehensive analysis of AMI patients, highlighting demographic shifts, risk factors, complications, and the effectiveness of rehabilitation programs. The 6MWT emerges as a valuable tool for prognostic assessment, emphasizing its safety and adaptability in various contexts. We posit recommendations to integrate the 6MWT into standard post-AMI care, emphasizing its role in predicting prognosis. Additionally, a focus on rehabilitation programs for better outcomes is advised.
In this study encompassing 71 Post-Myocardial Infarction (MI) patients, our findings illuminate the diverse dimensions of cardiovascular rehabilitation outcomes. Noteworthy demographic insights revealed a predominantly male and white population, with a peak age group of 50-69 years. A shift in BMI categories and a reduction in high-risk patients from 76% to 34.1% were observed between the first and second tests, accompanied by a decrease in mean BMI.
Chronic diseases were prevalent, affecting over 66% of the sample, with diabetes, hypertension, and their combination prominent. Complications post-MI, particularly heart failure, were identified in 25.4% during the second test. Treatment modalities demonstrated consistent coronary care unit management, encompassing medications and follow-up interventions such as angiography and PCI. Physiological assessments during walking tests showcased stable blood pressure and heart rate but significant improvement in oxygen saturation during the second test.
The most striking improvement was witnessed in the patients’ ability to cover distances, with all participants surpassing 400 meters in the second test, marking a substantial enhancement from the first test. Dyspnea levels decreased, and the majority completed the walking test without pauses. This study provides valuable insights into the effectiveness of cardiovascular rehabilitation, guiding efforts to optimize post-MI patient management and enhance recovery outcomes.
References
- What is cardiovascular disease? American Heart Association. 2022. www.heart.org/en/health-topics/consumer-healthcare/what-is-cardiovascular-disease.
- Katz D, Gavin MC. Stable Ischemic Heart Disease. Annals of internal medicine. 2019; 171: ITC17-ITC32. https://pubmed.ncbi.nlm.nih.gov/31382288/
- Victoria A. Effects of Altered Plasminogen Activator Inhibitor-1 Expression on Cardiovascular Disease. Curr Drug Targets. 2011; 12: 1782-1789. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3674863/
- William E. Optimal medical therapy with or without PCI for stable coronary disease. Cardiac assessment. 2007; 23: 1134- 1143. https://www.hsph.harvard.edu/wpcontent/uploads/sites/2448/2021/09/COURAGE-NEJM.pdf
- Sharp III TE. Drug and Cell-Based Therapies to Reduce Pathological Remodeling and Cardiac Dysfunction after Acute Myocardial Infarction. Temple University. 2017. https://scholarshare.temple.edu/handle/20.500.12613/2361.
- Bays HE, Taub PR, Epstein E, et al. Ten things to know about ten cardiovascular disease risk factors. American Journal of Preventive Cardiology. 2021; 100149. https://pubmed.ncbi.nlm.nih.gov/34327491/
- Katus H, Remppis A, Neumann F. Diagnostic efficiency of troponin T measurements in acute myocardial infarction. Circulation. 1991; 83: 902-912. https://pubmed.ncbi.nlm.nih.gov/1999039/.
- Apple F, Jaffe A. Cardiovascular disease. Fundamentals of clinical Chemistry. 2008; 6: 614-630.
- Bates E, Menees D. Acute ST-elevation myocardial infarction. Curr Opin Crit Care. 2012; 18: 417-423. https://pubmed.ncbi.nlm.nih.gov/22889871/
- Mujoomdar M, Russell E, Dionne F, et al. Optimizing Health System Use of Medical Isotopes and Other Imaging Modalities. Ottawa (ON): Canadian Agency for Drugs and Technologies in Health. 2012. APPENDIX 2.7, Assessment of Prognosis Post- Myocardial Infarction. https://pubmed.ncbi.nlm.nih.gov/24404637/.
- Hasanpour Dehkordi A, Ebrahimi-Dehkordi S, Banitalebi-Dehkordi F, et al. The effect of teach-back training intervention of breathing exercise on the level of dyspnea, six-minutes walking test and FEV1/FVC ratio in patients with chronic obstructive pulmonary disease; a randomized controlled trial. Expert Review of Respiratory Medicine. 2021; 15: 161-169. https://pubmed.ncbi.nlm.nih.gov/32921199/
- Dasari TW, et al. Prognostic value of 6-minute walk distance in patients undergoing percutaneous coronary intervention: A veterans affairs prospective study, Texas Heart Institute journal. 2020; 47(1): 10-14. doi: 10.14503/thij-17-6471. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7046352/#:~:text=assessment%2Fmethods%2C%20walking-,The%206%2Dminute%20walk%20distance%20(6MWD)%20test%20is%20a,admission%20in%20patients%20with%20HF.
- Agrawal MB, Awad NT. Correlation between six-minute walk test and spirometry in chronic pulmonary disease. Journal of clinical and diagnostic research: JCDR. 2015; 9: OC01. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4576573/.
- Costa HS, Lima MMO, Lage SM, et al. Six-minute walk test and incremental shuttle walk test in the evaluation of functional capacity in Chagas heart disease. Journal of exercise rehabilitation. 2018. https://pubmed.ncbi.nlm.nih.gov/30443532/
- Laboratories ATSC oP SfCPF. ATS statement: Guidelines for the sixminute walk test. Am J Respir Crit Care Med. 2002; 166(1): 111-117. https://pubmed.ncbi.nlm.nih.gov/12091180/.
- Steffen TM, Hacker TA, et al. Age- and gender-related test performance in community-dwelling elderly people: Six-Minute Walk Test, Berg Balance Scale, Timed up & Go Test, and gait speeds.” Physical Therapy. 2002; 82(2): 128-137. https://pubmed.ncbi.nlm.nih.gov/11856064/
- National Center for Health Statistics. Bridged-race inter censual estimates of the resident population of the United States for. 2009. https://www.cdc.gov/nchs/nvss/bridged_race.htm
- Xu Yao, Yi Jin, Chunlan Gao, Yuqin Zhang, Yun Lu, et al. (2023) Phase I cardiac rehabilitation with 5-phase music after emergency percutaneous coronary intervention for acute myocardial infarction: A prospective randomized study. Medicine. 2023; 102(9): e33183. https://pubmed.ncbi.nlm.nih.gov/36862883/.
- Patricia Angélica, De Miranda Silva NOGUEIRA, PT, Ana Cristina Monteiro LEAL, Cristiana PULZ, Ivan Daniel Bezerra NOGUEIRA, and Japy Angelini Oliveira FILHO. Clinical Reliability of the 6 Minute Corridor Walk Test. Performed Within a Week of a Myocardial Infarction. Int Heart J. 2006; 47(4): 533-540. https://pubmed.ncbi.nlm.nih.gov/16960408/.
- Ekman MJ, Klintenberg M, Björck U, Norström F, Ridderstråle M. Six-minute walk test before and after a weight reduction program in obese subjects. Obesity (Silver Spring). 2013; 21(3): E236-43. doi: 10.1002/oby.20046. PMID: 23404845. https://pubmed.ncbi.nlm.nih.gov/23404845/.
- Diniz LS, Neves VR, Starke AC, Barbosa MPT, Britto RR, et al. Safety of early performance of the six-minute walk test following acute myocardial infarction: a cross- sectional study. Braz J Phys Ther. 2017; 21(3):167-174. doi: 10.1016/j.bjpt.2017.03.013.
- Syifa Rahmani, Erwinanto, Rudolf Andean. Correlation between Six-Minutes’ Walk Test and Quality of Life in 471 Heart Failure Patients. Althea Medical Journal. 2015; 2. https://journal.fk.unpad.ac.id/index.php/amj/article/view/629.
- Sakir Arslan, Mustafa Kemal Erol, Fuat Gundogdu, Serdar Sevimli, Enbiya Aksakal, et al. Prognostic Value of 6-Minute Walk Test in Stable Outpatients with Heart Failure. Tex Heart Inset J. 2007; 34: 166-9. https://pubmed.ncbi.nlm.nih.gov/17622362/.
- BJ Witt, et al. Cardiac rehabilitation after myocardial infarction in the community. J Am Coll Cardiol. 2004. https://pubmed.ncbi.nlm.nih.gov/15337208/.
- PR Lawler, et al. Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: A systematic review and meta-analysis of randomized controlled trials Am Heart J. 2001.
- TM Brown, et al. Predictors of cardiac rehabilitation referral in coronary artery disease patients: findings from the American Heart Association’s Get with the Guidelines Program J Am Coll Cardiol. 2009. https://pubmed.ncbi.nlm.nih.gov/21982647/.
- Shirley Aparecida Fabris de Souza, Joel Faintuch, Sonia Maria Fabris, Fernando Kenji Nampo, Cesar Luz, Thiago Lorena Fabio, Isabella Souza Sitta, Inês Cristina de Batista Fonseca, Six-minute walk test: functional capacity of severely obese before and after bariatric surgery, Surgery for Obesity and Related Diseases. 2009; 5. https://www.sciencedirect.com/science/article/pii/S1550728909004791
- Sousa PICP. Primária no enfarte de miocárdio com supradesnivelamento do segmento ST: Tempo para intervenc ¸ão e modos de referenciac ¸ão. Rev Port Cardiol. 2012. doi:10.1016/j.repc.2012.07.006. https://www.academia.edu/58848223/Primary_PCI_in_ST_elevation_myocardial_infarction_Mode_of_referral_and_time_to_PCI?uc-sb-sw=54272761.