Research Article
Volume 3, Issue 5
Prevalence, Types, Risk Factors, and Outcome of Congenital Malformations in Two Health Facilities in the South West Region of Cameroon
Yolande Djike PF1*; Charlotte Eposse2 ; Winifred N Abanda3 ; Yanelle Wandji1 ; Diomède N Njinkui4 ; Naiza Monono4 ; Godlove K Jator6 ; Andreas Chiabi6
1Faculty of Health Sciences, University of Buea, Regional Hospital Buea, Cameroon.
2Faculty of Medicine and Pharmaceutical Sciences, University of Douala, Cameroon.
3Faculty of Health Sciences, University of Buea, Cameroon.
4Faculty of Medicine and Pharmaceutical Sciences, University of Dschang, Cameroon.
5Faculty of Health Sciences, University of Buea, Regional Hospital Limbe, Cameroon.
6Faculty of Medicine and Pharmaceutical Sciences, Health Sciences, University of Bamenda, Cameroon.
Corresponding Author :
Yolande Djike PF
Email: yolandep2000@yahoo.fr
Received : Apr 26, 2024 Accepted : May 20, 2024 Published : May 27, 2024 Archived : www.meddiscoveries.org
Citation: Djike PFY, Eposse C, Abanda WN, Wandji Y, Njinkui DN, et al. Prevalence, Types, Risk Factors, and Outcome of Congenital Malformations in Two Health Facilities in the South West Region of Cameroon. Med Discoveries. 2024; 3(5): 1158.
Copyright: © 2024 Djike PFY. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background: Birth defects also known as congenital abnormalities are structural or functional anomalies that occur during intrauterine life and can be identified prenatally, at birth, or be detected later in infancy. Due to paucity of information on congenital malformations in developing countries, we aimed to determine the prevalence, risk factors and outcome of congenital malformations among neonatal admissions in the Buea and Limbe Regional Hospitals.
Methods: A hospital-based case control study in which a review of the records of all neonates admitted in the pediatric unit of the Buea and Limbe Regional Hospitals over a 6-year period (1st of January 2017 to the 31st of December 2022) was conducted. An extraction sheet was used to retrieve information from the patient’s file who met up with the inclusion criteria. Data was entered in excel and analyzed using the Statistical Package for Social Sciences (SPSS) version 26.
Results: Overall prevalence of congenital malformations in our study was of 2.6%. The risk factors identified were area of residence (OR=3.39, CI=1.32-8.69, p=0.011), antenatal visits <8 times (OR=4.34, CI=1.38-13.58, p=0.012), mothers who took artesunate (OR=0.34 CI=0.14-0.87, p=0.024), peri-conceptional folic acid at 12-28 weeks (OR=2.12, CI=1.09-4.13, p=0.028) and those who started at >28 weeks (OR=16.41, CI=1.94-138.95, p=0.010). There was no significant association between congenital malformations and birth weight, maternal age, occupation, marital status and parity. The most common types where malformations of the musculoskeletal system. Majority of cases were referred (39%) and 14% died.
Conclusion: There was a high prevalence of congenital malformations in our study. Risk factors such as antenatal attendance, area residence, and time of start of peri-conceptional folic acid greatly contributed to the high prevalence of congenital malformations. Majority of neonates ended up being referred with the cases involving the cardiovascular system. Therefore, there is need to establish a surveillance system for congenital malformations and efforts should be made to create awareness on the risk factors.
Keywords: Congenital malformation; outcome; Urban; Rural.
Introduction
Congenital malformations are structural and functional anomalies that occur during intrauterine life and these conditions develop prenatally and can be identified before, at birth or later in life [1]. An estimated 7.9 million children worldwide are born with congenital malformations yearly [1]. Approximately 25% of pediatric hospital admissions and about onethird of the total number of pediatric hospital days are for congenital malformations of various types [2]. Etiologies of birth defects is documented to be multifactorial and these includes genetic disorders, poor nutrition, TORCH infections (toxoplasmosis, others (syphilis, varicella zoster), rubella, cytomegalovirus, herpes simplex virus), ingestion of alcohol, and exposure to environmental pollutants such as pesticides, tobacco use, maternal venereal diseases, advanced maternal age, and medical disease conditions in the mothers [3]. About 50% of congenital malformations have not been ascribed to any known etiology [4]. Congenital malformations affects several organ-system and this depends on the stage of embryogenesis when the insult occurred [5]. Some studies have reported central nervous system anomalies as the most predominant congenital malformation [6], while others have reported abnormalities of the cardiovascular system [7]. Few studies have been conducted on the prevalence, risk factors, and outcome of congenital malformations in Cameroon.
Methods
This study was carried out in the neonatology unit of the Buea and Limbe Regional Hospitals in the Fako Division of the South West Region of Cameroon. These are the two principal secondary health facilities which serve as the main referral hospitals in the South West Region and provides multi-specialist care. The neonatology unit which is being headed by Pediatricians. This unit provides care for neonates born within and outside the hospital, alongside specialized care such as phototherapy, incubator and Kangaroo Mother care method.
Study design
This was a hospital based 6-year retrospective case-control study. This 6 year retrospective case-control study was conducted over a period of 3 months from February 2023 till April 2023. The 6 year period studied, was from January 1st 2017 till December 31st 2022. The study population included all files of neonates (0-28 days) admitted in the Buea and Limbe.
Regional hospitals within the study period
Data collection: All files of neonates admitted in the pediatric unit from January 1st 2017 to December 31st 2022 were retrieved for the study, from which cases and controls were selected and matched for same sex, gestational age ± 3 weeks and of the same region of origin. Cases were neonates with congenital malformations and controls were neonates without congenital malformations. Through convenient sampling a minimum sample size of 95 cases was calculated using the Schlesselman formula for cases-control studies. Cases and controls were selected in a ratio of 1:1 and matching was done based on the sex of the neonate, gestational age ± 3 weeks, and mothers region of residence. All cases of still births with congenital malformations and neonates with 30% of missing data were excluded.
Data management and analysis: Data collected coded and entered into excel sheet and later exported and analyzed using Statistical Package for Social Sciences version 26 (SPSS).
Categorical variables were summarized using frequencies, and percentages, along with a 95% confidence interval. Continuous variables were summarized using mean and standard deviation. Associated factors were analyzed using bivariate and multivariate analysis. Independent variables: Maternal age, socioeconomic status, educational background, maternal health status, maternal exposure to infections, medications, tobacco, alcohol, mode of deliver, gestational age, sex, and birth weight of the neonates. Dependent variables: Types of congenital malformations, outcome. The prevalence rate of congenital malformation was calculated as the proportion of neonates with congenital malformation over the total number of neonates admitted during the study period. Associations of neonatal characteristics and maternal socio-demographic factors with congenital malformations between cases and controls were analyzed using binary and multiple logistic regressions. Risk factors with p-values <0.05 were on bivariate analysis were entered into multivariate logistic regression model to evaluate the association between the risk factors and CM. CM were classified according to ICD-10 (International classification of Diseases-10).
Ethical clearance
Ethical approval was obtained from the institutional review board of the Faculty of Health Science, (Ref: 2023/1993-02/UB/ SG/IRB/FHS) University of Buea, while administrative authorization was obtained from the Southwest Regional Delegation of Public health and the Director of the Buea Regional Hospital. This study was carried out strictly for scientific purposes only and not to generate any profit. The data collected was handled properly so as to maintain patient’s confidentiality.
Results
A total of 4396 records of patients admitted at the neonatology unit within the 6-year period were retrieved, of which 115 cases of congenital malformations were retained. Among the cases, 15 files were excluded due to insufficient data. So 100 cases and, 100 controls were selected and matching was done based on the sex of the neonate, gestational age ± 3 weeks, and mothers region of residence.
Characteristics of the study population distribution of characteristics of the neonates
Majority of neonates with congenital malformations were diagnosed postnatal 93(93%), 71(71%) were term neonates and the majority of neonates were males 58(58%) with a sex ratio of 1:4. Also, 59(59%) of neonates were born through vaginal delivery with many neonates weighing from 2500 g - 4000 g 79(79%). Majority of cases were referred from other hospitals and 56% came in for consultation or were transferred from the maternity.
Socio-demographic characteristics of the mother
Maternal ages of neonates with malformations ranged from 17 to 43 years, with a mean of 28.1±5.4 years and 82(82%) were aged 20-34 years. More than half of the mothers were employed, 35(35%) were unemployed. Majority of the mothers resided in urban settings, while 19(19%) resided in rural areas. Majority of the mothers lived as couples 77(77%), while 23(23%) were single.
Prevalence of congenital malformations for each hospital
Table 1 shows the prevalence of congenital malformations in each hospital. Buea Regional Hospital had a higher prevalence of 4.2% than Limbe Regional Hospital with prevalence of 1.5%. With the 115 neonates admitted during the 6-year period, over all prevalence rate calculated was 2.6%.
Table 1: Prevalence for each hospital and overall prevalence for our study.
| Hospital | Total number of admissions |
Number of cases with Congenital malformations |
Prevalence (%) |
|---|---|---|---|
| Limbe | 2580 | 39 | 1.5 |
| Buea | 1816 | 76 | 4.2 |
| Total | 4396 | 115 | 2.6 |
Annual prevalence of congenital malformations in Buea regional hospital
The annual prevalence of congenital malformations in the Buea regional Hospital is demonstrated below, with highest prevalence occurring in the year 2022 (5.5%). There was a progressive increase in the prevalence of congenital malformations from 2019 to 2022 (Table 2).
Table 2: Annual prevalence rate in the Buea regional hospital.
| Years | Number of admissions |
Number of cases with congenital malformations |
Prevalence (%) |
|---|---|---|---|
| 2017 | 151 | 10 | 6.6 |
| 2018 | 295 | 5 | 1.7 |
| 2019 | 377 | 11 | 2.9 |
| 2020 | 288 | 15 | 5.2 |
| 2021 | 340 | 15 | 4.4 |
| 2022 | 365 | 20 | 5.5 |
Annual prevalence of congenital malformations in Limbe regional hospital
Regarding the pattern of prevalence of congenital in the Limbe regional hospital, 2022 had the highest prevalence (2.3%). The prevalence increased with time from 2017 till 2022 (Table 3).
Table 3: Annual prevalence rate in Limbe regional hospital.
| Years | Number of admissions |
Number of cases with congenital malformations |
Prevalence (%) |
|---|---|---|---|
| 2017 | 473 | 4 | 0.9 |
| 2018 | 369 | 3 | 0.8 |
| 2019 | 304 | 5 | 1.7 |
| 2020 | 392 | 5 | 1.3 |
| 2021 | 509 | 10 | 2.0 |
| 2022 | 533 | 12 | 2.3 |
Annual distribution of congenital malformations per year in both the Buea and Limbe regional hospitals
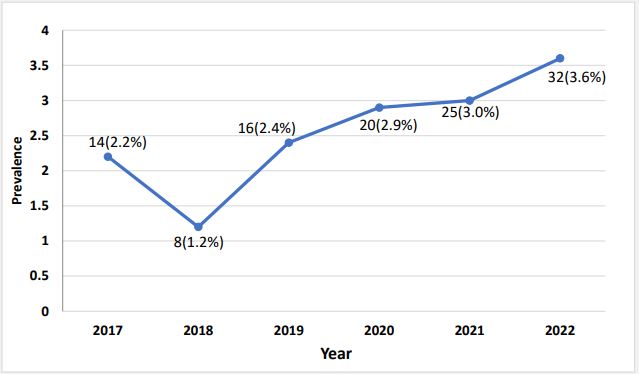
The annual prevalence of congenital malformations in both hospitals showed that, there was a progressive increase in the prevalence of congenital malformations from 2019 to 2022. The highest prevalence was found to be in 2022 (3.6%) (Figure 1).
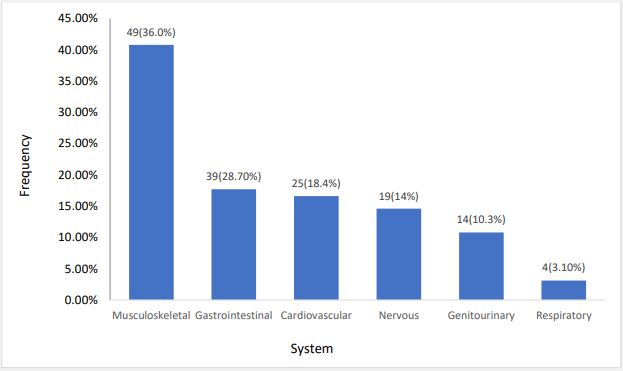
Classification according to systems
The most commonly affected system was the musculoskeletal system 49(36.0%), followed by gastrointestinal 39(28.7.7.1%) and Cardiovascular system 25(18.4%) (Figure 2).
Classification according to the International Classification of Diseases (ICD-10).
In the ICD-10 classification of congenital malformations, the most common system involved was the musculoskeletal system, with the most common type being omphalocele 7(25.9%) and talipes equinovarus 7(25.9), followed by the digestive sytem with the most common type imperforated anus 7(26.9%), the nervous system common type being Myelomeningocele 10(52.6%). The other systems involved were, the cardiovascular, genital, urinary, and eye, ear, neck and face, n=133 (Table 4).
Table 4: Classification according to the International Classifica- tion of Diseases (ICD-10).
| ICD codes |
Type of malformation | Frequen- cy (n) |
Percentage (%) |
|---|---|---|---|
| Q00-Q07 | Nervous system | ||
| Myelominigocele | 10 | 52.6 | |
| Microcephaly | 4 | 21.1 | |
| Congenital hydrocephalus | 5 | 26.3 | |
| Total | 19 | 100 | |
| Q10-Q18 | Eye, ear face and neck | ||
| Microphthalmia | 1 | 4.6 | |
| Ankyloblephroma | 1 | 4.6 | |
| Flat nasal bridge | 10 | 45.5 | |
| Low set ears | 10 | 45.5 | |
| Total | 22 | 100 | |
| Q20-Q28 | Circulator | system | |
| Ventricular septal defect | 5 | 23.8 | |
| Transposition of the great arteries | 4 | 19.1 | |
| Patent ductus arteriosus | 3 | 14.3 | |
| Atrial septal defect | 2 | 9.5 | |
| Dilated ventricles | 2 | 9.5 | |
| Tricuspid artresia | 1 | 4.8 | |
| Patent foramen ovale | 1 | 4.8 | |
| Coarctation of the aorta | 1 | 4.8 | |
| Tetralogy of fallot | 1 | 4.8 | |
| Small vena cava | 1 | 4.8 | |
| Total | 21 | 100 | |
| Q30-Q34 | Respiratory system | ||
| Choanal atresia | 2 | 50 | |
| Nasal cleft | 1 | 25 | |
| Laryngomalacia | 1 | 25 | |
| Total | 4 | 100 | |
| Q35-Q37 | Cleft lip and palate | ||
| Complete cleft lip and palate | 3 | 10 | |
| Q38-Q45 | Digestive system | ||
| Impeforated anus | 7 | 26.9 | |
| Tracheoesophageal fistula | 3 | 11.5 | |
| Hypertrophic pyloric stenosis | 3 | 11.5 | |
| doudenal atresia | 3 | 11.5 | |
| Jejunal atresia | 2 | 7.7 | |
| Topus palatinus | 2 | 7.7 | |
| Perianal fistula | 2 | 7.7 | |
| Esophageal atresia | 2 | 7.7 | |
| Vestibular fistula | 1 | 3.9 | |
| Ileal atresia | 1 | 3.9 | |
| Total | 26 | 100 | |
| Q50-Q56 | Genital organs | ||
| Cryptochidism | 8 | 80 | |
| Congenital Hydrocele | 2 | 20 | |
| Total | 10 | 100 | |
| Q60-Q64 | Urinary system | ||
| Polycystic kidney | 2 | 50 | |
| Posterior urethral valve | 2 | 50 | |
| Total | 4 | 100 | |
| Q65-Q79 | Musculoskeletal system | ||
| Omphalocele | 7 | 25.9 | |
| Talipes equinovarus | 7 | 25.9 | |
| Polydactyly | 6 | 22.2 | |
| syndactyly | 2 | 7.4 | |
| Prune belly | 2 | 7.4 | |
| Congenital diastasis | 1 | 3.7 | |
| Arthrogyposis congenita | 1 | 3.7 | |
| Genu varum | 1 | 3.7 | |
| Total | 27 | 100 | |
| Q80-Q89 | Others | 0 | 0.0 |
| Q90-Q99 | Chromosomal abnormalities | 0 | 0 |
Risk factors for congenital malformations
Socio-demographic characteristics of the mother and congenital malformations: Of the factors analyzed, residing in a rural setting significantly increased the chances of having a child with a congenital malformation (OR=3.12; CI 95% (1.25-7.79); p=0.015). Mothers of cases were slightly older than mothers of controls but the difference was not statistically significant. Occupation and marital status were not significantly associated with the occurrence of congenital malformations (Table 5).
Obstetric factors associated with congenital malformations: Attending less than 8 antenatal consultations (OR=4.43; CI; p=0.010) was associated with increased chance of congenital malformations. Mothers who attended <8 Antenatal consultation were 4 times more likely to have newborns with congenital malformations than those who attended >8 times. Mothers of cases were more multipara and some did not attend antenatal consultations compared to the controls but this difference was not statistically significant (Table 6).
Pathologies during pregnancy (first trimester): No factor analyzed was significantly associated to congenital malformations. With undefined odds ratios in multiple categories due to absence of exposure in the control group (Table 7).
Drugs taken during pregnancy: Starting periconceptional folic acid between 12-28 weeks significantly increased the risk of congenital malformations (OR=2.12; CI 95% (1.09-4.13); p=0.028), and those starting from 28 weeks and above have even higher chances of congenital malformations (OR=16.41; CI 95% (1.94-138.95); p=0.010) (Table 8).
Neonatal factors associated with congenital malformation: No significant association between birth weight and congenital malformations (Table 9).
Hospital outcome of neonates with congenital malformations: Mortality rate was 14%, those managed 21(21%) cases managed were mainly cases with gastrointestinal 9(42.8%) and musculoskeletal 9(42.9%) system malformations, those discharged 21(21%) were mainly musculoskeletal system malformations 12(57.1%), referred 39(39%) mainly cardiovascular system malformations 13(33.3%), discharged against medical advice (5%) mainly cardiovascular system malformations 2(40%) and died 14(14%) had mainly cardiovascular system malformations 5(35.7%) (Table 10).
Factors influencing survival in neonates with congenital malformations: The was no significant association between survival and age at diagnosis, Gestational age, Gender, mode of delivery, birth weight, frequency of antenatal, parity, and systems affected.
Table 5: Socio-demographic characteristics of the mother associated with congenital malformations (N=200).
| Variables | Cases | Controls | OR [95% CI] | p-value | Multivariate Logistic Regression | |||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | aOR [95% CI] | p-value | |||
| Age Group | ||||||||
| <20 | 6 | 6.0 | 5 | 5.0 | - | - | ||
| 20-34 | 82 | 82.0 | 84 | 84.0 | 0.81 [0.24-2.22] | 0.741 | 1.71 [0.40-7.23] | 0.468 |
| >34 | 12 | 12.0 | 11 | 11.0 | 0.91 [0.22-3.84] | 0.897 | 2.18 [0.39-12.11] | 0.371 |
| Area of Residence | ||||||||
| Urban | 81 | 81.0 | 93 | 93.0 | - | - | ||
| Rural | 19 | 19.0 | 7 | 7.0 | 3.12 [1.25-7.79] | 0.015 | 3.39 [1.32-8.69] | 0.011 |
| Occupation | ||||||||
| Employed | 65 | 65.0 | 69 | 69.0 | - | - | ||
| Unemployed | 35 | 35.0 | 31 | 31.0 | 1.20 [0.66-2.66] | 0.548 | 1.24 [0.64-2.38] | 0.524 |
| Marital Status | ||||||||
| Living as a couple | 77 | 77.0 | 83 | 83.0 | - | - | ||
| Single | 23 | 23.0 | 17 | 17.0 | 1.46 [0.73-2.94] | 0.290 | 1.61 [0.74-3.51] | 0.286 |
Table 6: Obstetrical factors associated with congenital malformations (N=200).
| Variables | Cases | Controls | OR [95% CI] | p-value | Multivariate Logistic Regression | |||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | aOR [95% CI] | p-value | |||
| Attended ANC | ||||||||
| Yes | 97 | 97.0 | 100 | 100.0 | - | - | ||
| No | 3 | 3.0 | 0 | 0.0 | - | - | ||
| Frequency of ANC | ||||||||
| <8 | 93 | 95.9 | 84 | 84.0 | 4.43 [1.42-13.77] | 0.010 | 4.34 [1.38-13.58] | 0.012 |
| ≥8 | 4 | 4.1 | 16 | 16.0 | - | - | ||
| Parity | ||||||||
| Primipara | 37 | 37.0 | 43 | 43.0 | 0.78 [0.44-1.37] | 0.387 | 0.77 [0.43-1.39] | 0.385 |
| Multipara | 63 | 63.0 | 57 | 57.0 | - | - | ||
Table 7: Pathologies during pregnancy in the first trimester and association with congenital malformations.
| Pathologies | Cases | Controls | OR [95% CI] | p-value | ||
|---|---|---|---|---|---|---|
| N | % | N | % | |||
| Rubella | 1 | 1.0 | 0 | 0.0 | - | |
| Toxoplasmosis | 4 | 4.0 | 0 | 0.0 | - | |
| Malaria | 13 | 13.0 | 23 | 23.0 | 0.50 [0.24-1.06] | 0.069 |
| Chlamydia | 1 | 1.0 | 2 | 2.0 | 0.49 [0.04-5.55] | 0.568 |
| Syphilis | 2 | 2.0 | 1 | 1.0 | 2.02 [0.18-22.65] | 0.568 |
| Oligohydramnios | 4 | 4.0 | 0 | 0.0 | - | |
| Polyhydramnios | 3 | 3.0 | 0 | 0.0 | - | |
Table 8: Drugs taken during pregnancy and association with congenital malformations.
| Drugs | Cases | Controls | OR [95% CI] | p-value | Multivariate Logistic Regression |
|||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | aOR [95% CI] | p-value | |||
| Time of start periconceptional folic acid | ||||||||
| <12 | 19 | 19.6 | 38 | 38.0 | - | - | ||
| 12-28 | 68 | 70.1 | 61 | 61.0 | 2.23 [1.16-4.27] | 0.016 | 2.12 [1.09-4.13] |
0.028 |
| >28 | 10 | 10.3 | 1 | 1.0 | 20.00 [2.38-167.98] | 0.006 | 16.41 [1.94-138.95] |
0.010 |
Table 9: Association between birth weight and congenital malformations.
| Birth weight | Cases | Controls | OR [95% CI] | p-value | Multivariate Logistic Regression |
|||
|---|---|---|---|---|---|---|---|---|
| N | % | N | % | aOR [95% CI] | p-value | |||
| <1500 | 2 | 2.0 | 1 | 1.0 | 3.00 [0.22-40.93] | 0.410 | 2.16 [0.12-39.64] | 0.604 |
| 1500-2499 | 13 | 13.0 | 4 | 4.0 | 4.88 [1.06-22.38] | 0.042 | 2.13 [0.28-15.96] | 0.462 |
| 2500-4000 | 79 | 79.0 | 86 | 86.0 | 1.38 [0.47-4.05] | 0.560 | 1.47 [0.43-5.04] | 0.537 |
| >4000 | 6 | 6.0 | 9 | 9.0 | - | - | ||
Table 10: Association between birth weight and congenital mal- formations.
| Hospital admission outcome |
Systems involved | Frequencies | Percentages (%) |
|---|---|---|---|
| Discharged | Musculoskeletal | 12 | 57.1 |
| Gastrointestinal | 3 | 14.3 | |
| Nervous | 3 | 14.3 | |
| Genitourinary | 3 | 14.3 | |
| Total | 21 | 100 | |
| Managed | Musculoskeletal | 9 | 42.9 |
| Gastrointestinal | 9 | 42.9 | |
| Genitourinary | 3 | 4.3 | |
| Total | 21 | 100 | |
| Referred | Cardiovascular | 13 | 33.3 |
| Gastrointestinal | 12 | 30.8 | |
| Nervous | 11 | 28.2 | |
| Musculoskeletal | 2 | 5.1 | |
| Respiratory | 1 | 2.6 | |
| Total | 39 | 100 | |
| Discharged against medical advice |
Cardiovascular | 2 | 40 |
| Nervous | 1 | 20 | |
| Musculoskeletal | 1 | 20 | |
| Musculoskeletal | 1 | 20 | |
| Total | 5 | 100 | |
| Died | Cardiovascular | 5 | 35.7 |
| Nervous | 3 | 21.4 | |
| Musculoskeletal | 3 | 21.4 | |
| Gastrointestinal | 1 | 7.1 | |
| Respiratory | 1 | 7.1 | |
| Genitourinary | 1 | 7.1 | |
| Total | 14 | 100 |
Discussion
Overall prevalence of CM in this study was 2.6%. Nguefack et al. in Douala in 2015, noted a low prevalence of 1.64% [9]. However a prevalence of 9.0% was recorded by Kamla et al., in Yaounde in 2017 [10]. We observed a higher prevalence (4.2%) of congenital malformation in the Buea Regional Hospitals than in the Limbe Regional Hospitals with a prevalence of 1.5%. This is due to the fact that Buea Regional Hospital is located in the heart of the South West region, and it is a specialized hospital embedded with necessary facilities for better management of these newborns.
The most common affected systems involved according to the classification by systems and according to the WHO International Classification of Diseases (ICD-10), were the musculoskeletal and gastrointestinal systems. The most common types were Omphalocele (7), talipes equinovarus (7), imperforated anus (7), myelomeningocele (10), and cryptorchidism (8). This finding was similar to those reported by Nguefack et al. in 2015 in Douala [9], Kamla et al. in 2017 in Yaounde [10], Forci et al. in Morocco in 2020 [11]. The cardiovascular system was reported in Nigeria by Ajao et al. in 2019 [12] and South Africa by Saib et al. in 2021 [13].
Of the factors analyzed and after multivariate analysis with logistic regression, congenital malformations were associated with area of residence, number of antenatal consultations, and time of start of periconceptional folic acid. Mothers who resided in rural areas were significantly associated with having babies with congenital malformation. Mothers who lived in rural areas lacked well equipped health facilities for proper follow up and education during the antenatal period. This was similar to a study carried out in Iran by Rayahifar et al. in 2021 [16]. A study conducted in Egypt by Shalaby et al. revealed that the risk of having malformations occur in those who lived urban areas than rural areas due to the risk of exposure to environmental pollution in the urban areas [17].
Mothers who attended Antenatal Consultations (ANC) less than 8 were 4 times more likely to have babies who had congenital malformations than those who attended more than 8 times. Mothers who attended antenatal <8 times had less follow-up since during antenatal visits health education is usually given on various issues including adequate and healthy nutrition, and preventive, screening and curative measures are carried out. This was similar to a study carried out by Birhanu et al in Ethopia, 2021 [18], where inadequate antenatal consultations was a risk factor for congenital malformations.
Mothers who took folic acid from 12-28 weeks were significantly associated with congenital malformations and mothers who took folic acid at >28 weeks were even more likely to have newborns with congenital malformations. Folic acid is necessary for early fetal development, and has been linked to cause malformations such as neural tube defects. Lack of folic acid in early pregnancy can lead to these malformations. This finding is in line with a study reported by Birhanu et al. in Ethopia in 2021 [15] and Abebe et al. in Nigeria [16], where all pregnant women who took folic acid in early pregnancy were where less likely to have babies with congenital malformations.
Majority of neonates with congenital malformations were referred (39%), to tertiary health facilities for specialist management and the most common malformations referred were malformations of the cardiovascular system 37.1%. Only 21% were managed which were mainly malformations of the gastrointestinal system and musculoskeletal system malformations were the most common malformations discharged this may be due to the fact that some were minor malformations which were not life threatening. Some left the hospital against medical advice (5%), this could be related to the stigmatization associated with having a malformed baby and may also be due to financial constraints. The highest number of neonates who died was cases with cardiovascular system malformations. The overall mortality rate due to congenital malformations was 14%. This was similar to a study carried out by Ajao et al. in Nigeria who had a mortality rate of 10.4% [12].
Age at diagnosis, gestational age, Gender, mode of deliver, birth weight, frequency of antenatal, parity and systems affected were not significantly associated with survival in neonates with congenital malformations. This was similar to a study conducted by Anane et al. [17].
However some limitations of the study were noted. The results may not be generalized to the general population given that this was a hospital-based study. This study was based on previously collected data, hence some missing data could not be recovered, adequate information on some obstetrics history and maternal risk factors could not assessed. Also, outcomes after discharge or referral could not be determined.
Conclusion
The overall prevalence of congenital malformations in our study was 2.6%. The most common malformations observed were the musculoskeletal system followed by the gastrointestinal and the cardiovascular system. Risk factors for CM were the area of residence, the number of antenatal consultations, and time of start of periconceptional folic acid. Majority of the cases with congenital malformations were referred (35%), 19% were managed and 14% died. Concluding these, pregnant women should be encouraged to do the recommended monitoring of ANC, and to start taking folic acid in the first trimester or as soon as the pregnancy is diagnosed.
Funding: These research did not receive any specific grant from funding agencies in the public, commercial, or not-forprofit sectors.
Declaration of competing interest: None.
References
- Geneva: World Health Organization. Congenital disorders. World Health Organ. 2023. https://www.who.int/news-room/fact- sheets/detail/birth-defects.
- Centres for Disease Control and Prevention. Causes of Congenital Anomalies and Classification According to Developmental Mechanism and Clinical Presentation. Centers for Disease Control and Prevention. 2020. https://www.cdc.gov/ncbddd/birthdefects/surveillancemanual/appendices/appendix-c.html
- Toufaily MH, Westgate MN, Lin AE, Holmes LB. Causes of Congenital Malformations. Birth Defects Res. 2018; 110(2): 87-91.
- Enow Orock G, Weledji EP, Egbe T, Halle Ekane EG, Ngowe NM. Congenital Malformations: Report of 5 Rare Cases Seen in 20 Years (1994-2014) in Cameroon and Review of Literature. Afr J Integr Health. 2015; 5: 6.
- Van der Bie G. Embryology. Early development from a Phenomenological point of view. Louis Bolk Institute. 2001.
- Djientcheu V de P, Njamnshi AK, Wonkam A, Njiki J, Guemse M, et al. Management of neural tube defects in a Sub-Saharan African country: The situation in Yaounde, Cameroon. J Neurol Sci. 2008; 275(1): 29-32.
- Chimah OU, Emeagui KN, Ajaegbu OC, Anazor CV, Ossai CA, et al. Congenital malformations: Prevalence and characteristics of newborns admitted into Federal Medical Center, Asaba. Health Sci Rep. 2022; 5(3): e599.
- Charlotte TN, Aurore ND, Charlotte B, Esther B, Eugene BP. Prenatal Diagnosis of Congenital Malformations in Douala General Hospital. Open J Obstet Gynecol. 2015; 5(15): 839-48.
- Kamla JI, Kamgaing N, Fongang EN, Fondop J, Billong S, et al. Epidémiologie des Malformations Congénitales Visibles à la Naissance à Yaoundé. Health Sci Dis. 2017; 18(4).
- Forci K, Alami MH, Bouaiti E, Slaoui M, Mdaghri Alaoui A, et al. Prevalence of congenital malformations at the les Orangers maternity and reproductive health Hospital of Rabat: descriptive study of 470 anomalies. BMC Pediatr. 2020; 20(1): 272.
- Ajao A, Adeoye I. Prevalence, risk factors and outcome of congenital anomalies among neonatal admissions in OGBOMOSO, Nigeria. BMC Pediatr. 2019; 19.
- Saib MZ, Dhada BL, Aldous C, Malherbe HL. Observed birth prevalence of congenital anomalies among live births at a regional facility in KwaZulu Natal Province, South Africa. PLoS ONE. 2021; 16(8): e0255456.
- Riyahifar S, Khoei RAA, Mirnia K. Contribution Factors on Congenital Malformations in Neonates in Iran. Iran J Pediatr. 2021; 31(5).
- Shalaby AM, EL-Gazzar AF. The Frequency, Types and Risk Factors of Congenital Anomalies in a Tertiary Neonatal Intensive Care Unit (A hospital based study). Ann Neonatol J. 2021; 3(1): 24-45.
- Birhanu K, Tesfaye W, Berhane M. Congenital Anomalies in Neonates Admitted to a Tertiary Hospital in Southwest Ethiopia: A Cross Sectional Study. Ethiop J Health Sci. 2021; 31(6): 1155-62.
- Abebe S, Gebru G, Amenu D, Mekonnen Z, Dube L. Risk factors associated with congenital anomalies among newborns in southwestern Ethiopia: A case-control study. PLOS ONE. 2021; 16(1): e0245915.
- Anane-Fenin B, Opoku DA, Chauke L. Prevalence, Pattern, and Outcome of Congenital Anomalies Admitted to a Neonatal Unit in a Low-Income Country-a Ten-Year Retrospective Study. Matern Child Health J. 2023; 27(5): 837-49.