Short Report
Volume 3, Issue 5
Vulvar Angiokeratoma after Radical Hysterectomy and Radiotherapy: Case Report
Hamraoui Hafsa*; Elloudi Sara; Baybaye Hanane; Soughi Meryem; Douhi Zakia; Mernissi Fatima Zahra
Department of Dermatology - Hassan II University Hospital Center of Fez, Morocco.
Corresponding Author :
Hamraoui Hafsa
Tel: +212-6-49-91-33-85;
Email: Hamraoui.hafsa@usmba.ac.ma
Received : Apr 01, 2024 Accepted : May 16, 2024 Published : May 23, 2024 Archived : www.meddiscoveries.org
Citation: Hafsa H, Sara E, Hanane B, Meryem S, Zakia D, et al. Vulvar Angiokeratoma after Radical Hysterectomy and Radiotherapy: Case Report. Med Discoveries. 2024; 3(5): 1156.
Copyright: © 2024 Hafsa H. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Angiokeratomas are relatively rare vascular malformations, whose surface is keratotic and located at the vulvar level called Fordyce angiokeratoma. We report the case of a vulvar angiokeratoma post hysterectomy and radiotherapy.
Keywords: Blood vessels; Hemangioma; Skin tumors.
Introduction
Angiokeratomas characterized by numerous dilated vessels in the superficial dermis with epidermal hyperplasia and hyperkeratosis [1]. It is generally observed on the scrotum and can rarely involve the vulva [2] the overall prevalence of angiokeratomas has been documented at 0.16% [3]. The true incidence of vulvar angiokeratoma in the general population is unknown. We report here the case of a patient in who was diagnosed with vulvar angiokeratoma after radical hysterectomy and radiotherapy.
Observation
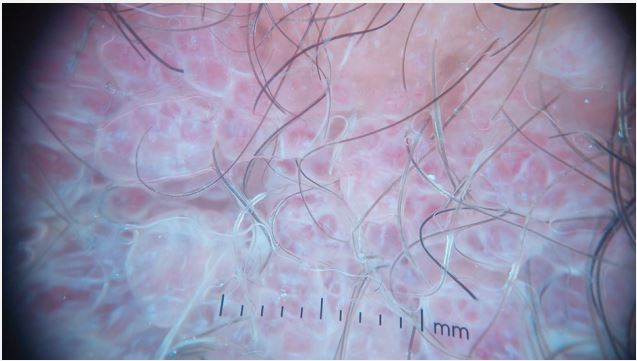
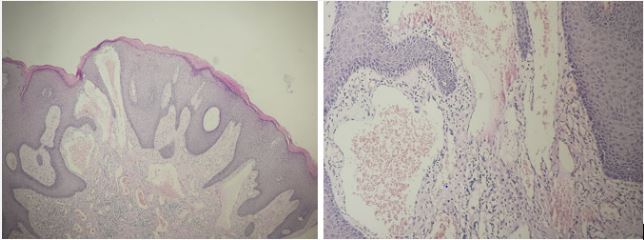
This is a 54-year-old patient with a history of squamous cell carcinoma of the cervix 12 years ago, treated by hysterectomy with bilateral iliac dissection, radiotherapy and chemotherapy. Her history of the disease goes back 2 years when the lesions appeared. Pruritic at the genital level, on dermatological examination we note the presence of a polylobed erythematous plaque made of small papule and translucent confluence at the level of the two labia majora on the dermoscopic level we note the presence of pink lacunae and a white veil (Figures 1 and 2) a biopsy was taken revealing a papillomatous epidermis surmounted by an ortho keratotic hyperkeratosis with numerous dilated vessels at the level of the papillary dermis concluding in an angiokeratoma (Figure 3). The patient received her first laser session.
Discussion
Vulvar angiokeratomas are generally unilateral, appearing mainly on the labia majora particularly in premenopausal women [4]. They can cause symptoms and consist of small benign vascular tumors with papular, nodular or warty morphology, purple or pink in color [5]. The dermoscopic signs suggestive of angiokeratoma are not very specific in isolation but include the presence of red to purplish ovoid lacunae, a white veil partially covering the lesion, as in the case of our patient, peripheral halo erythema, sometimes hemorrhagic crusts [6]. Histologically, these are dilated subepidermal vessels, associated with epidermal hyperplasia such as acanthosis or hyperkeratosis [7]. These lesions are generally asymptomatic, but can bleed, thrombose, or be traumatized. Various factors involved in the pathogenesis of angiokeratoma of the vulva include the use of contraceptive pills, localized venous hypertension due to varicocele, obesity and phlebectasia associated with chronic inflammation, radiotherapy and hysterectomy, pregnancy [8], our patient had a hysterectomy with bilateral iliac dissection which can lead to an increase in venous pressure and secondary vascular dilatation in addition to radio-induced damage to venous blood vessels. These factors are all known to contribute to the development of angiokeratomas. Vulvar angiokeratoma poses a problem of differential diagnosis with condylomata and intraepithelial neoplasia, which is why the final diagnosis is not clinical; it is always made by the pathologist [9].
Many treatments have been proposed ranging from therapeutic abstention, surgical excision, cryotherapy, electrocoagulation, radiofrequency, sclerotherapy, lasers including the erbium, diode, CO2 and Nd yag laser [10-12].
Conclusion
Because vulvar angiokeratoma is rare, it is often misdiagnosed as genital warts or a malignant vascular tumor. Radiotherapy increases the risk after a hysterectomy and lymph node dissection, the dermoscope guides the diagnosis but requires histological confirmation, hence the interest in a comparison between anamnesis, good clinical examination and dermoscopic analysis.
Conflict of interest: The authors declare that they have no conflicts of interest.
References
- Fogagnolo L, Cintra ML, Velho PENF. Angiokeratoma of the vulva. A Dermatol Arm. 2011; 86(2): 333-5.
- Bhagan LB, Knaus JV. Concurrent diagnosis of vulvar angiokeratoma with recurrent squamous cell carcinoma after radical vulvectomy and radiation therapy. Gynecol Oncol Case Rep. 2012; 2(3): 80-2.
- Naranjo-Sintes R, Pereda-Hernandez P, Delgado-Florencio V, Linares-Solano J. Angioqueratoma: A Proposito de 93 Observaciones.Méd. Cutaneous. Ibero Lat. Am.1988; 16(3): 255-261.
- Kontogianni-Katsaros K, Kairi-Vassilatoy E, Grapsa D, Papadias K, Hasiakos D, et al. Angiokeratoma of the vulva: A rare benign vascular tumor mimicking malignancy - case reports. EUR. J. Gynaecol. Oncol. 2006; 27(6): 632-633.
- Haidopoulos DA, Rodolakis AJ, Elsheikh AH, Papaspirou I, Diakomanolis E. Vulvar angiokeratoma following radical hysterectomy and radiotherapy. Acta Obstet Gynecol Scand. 2002; 81(5): 466-7.
- Zaballos P, Daufí C, Puig S, Argenziano G, Moreno-Ramírez D, et al. Dermoscopy of solitary angiokeratomas: A morphological study. Arch Dermatol. 2007; 143: 318‑25.
- Dhawan AK, Pandhi D, Goyal S, Bisherwal K. Angiokeratoma of vulva mimicking genital warts. J Obstet Gynaecol India. 2014; 64(Suppl 1): 148-9.
- Deo K, Dash KN, Sharma YK, Wadhokar M, Gupta A. Acquired angiokeratomas of the vulva. Indian J Sex Transm Dis. 2018; 39: 136-8.
- Bhandari V, Naik A, Gupta KL, Kausar M. Radiation-induced Vulvar Angiokeratoma Along with Other Late Radiation Toxicities after Carcinoma Cervix: A Rare Case Report. Indian J Dermatol. 2016; 61(2): 235.
- Samudrala S, Bhat MR. Recurrent nodular lesions on the vulva: A diagnostic challenge. Indian J Sex Transm Dis. 2018; 39: 124-6.
- T Badri, S Bouchouicha, H Hammami, J El Khalifa, S Ben Jennet, et al. Treatment of genital angiokeratomas by long pulse Nd: YAG laser: Study of 12 cases. Annals of Dermatology and Venereology. 2014; 141: 6-7, Supplement 1: S58.
- Sahu P, Kalra KD, Dayal S, Goyal P. Sclerotherapy in Angiokeratoma of the Vulva: A Cost-Effective Approach. Dermatol Surg. 2020; 46(1): 142-144.