Research Article
Volume 3, Issue 5
A Cross–Sectional Study on HIV Positive Mothers and Infant Feeding: Paradigm of Choices in a Regional Hospital in Cameroon
Pisoh W Dobgima1,2*; Petra N Kana1; Achuo Ascensius Ambe Mforteh1,2,3; Samuel A Angwafor1,2; Joel M Ngum4; Felister Sevidzem5; Andreas Chiabi1
1Faculty of Health Sciences, University of Bamenda, Bamenda, Cameroon.
2Bamenda Regional Hospital, Bamenda, Cameroon.
3Nkwen Baptist Hospital, Bamenda, Cameroon.
4Nkwen District Hospital, Bamenda, Cameroon.
5St. Blaise Catholic Hospital, Bamenda, Cameroon.
Corresponding Author :
Pisoh Walter Dobgima
Tel: +237-677368454;
Email: dobpisoh@yahoo.co.uk
Received : Mar 25, 2024 Accepted : May 06, 2024 Published : May 13, 2024 Archived : www.meddiscoveries.org
Citation: Dobgima PW, Kana PN, Mforteh AAA, Angwafor SA, Ngum JM, et al. A Cross–Sectional Study on HIV Positive Mothers and Infant Feeding: Paradigm of Choices in a Regional Hospital in Cameroon. Med Discoveries. 2024; 3(5): 1153.
Copyright: © 2024 Dobgima PW. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objective: The general objective of this study was to identify the infant feeding choices of HIV-positive mothers in four hospitals in the Bamenda Health District.
Materials and methods: This was a cross-sectional analytic study which was done for 5 months in the Bamenda Regional Hospital, Nkwen Baptist Hospital, Nkwen District Hospital and St. Blaise Catholic Hospital. Logistic regression analysis was used to assess the factors associated to infant feeding choice with statistical significance set at a p-value <0.05 with a 95% confidence interval.
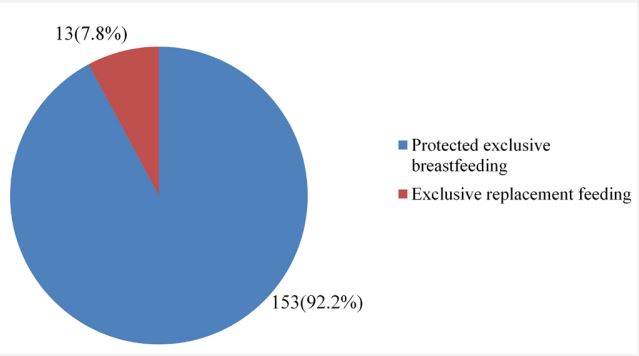
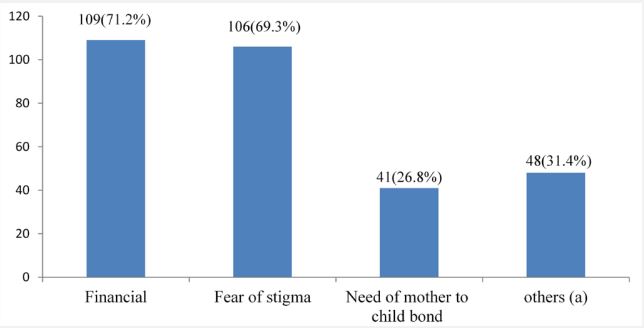
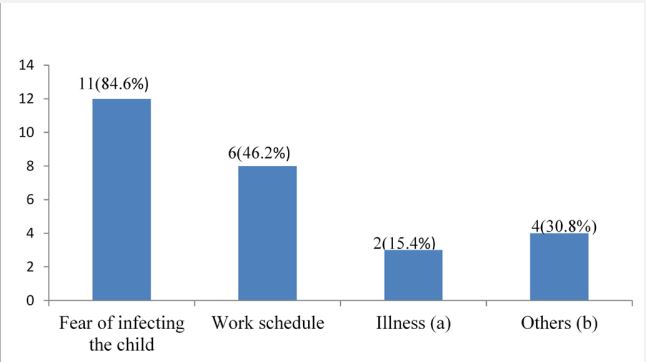
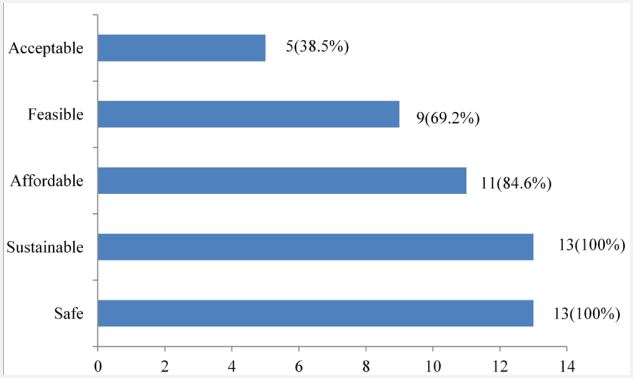
Results: Of the 166 participants included in our study, the prevalence of Exclusive BreastFeeding (EBF) was found to be 92.2% and Exclusive Replacement Feeding (ERF) was 7.8%. The main reasons for choosing EBF were found to be financial constraint and fear of stigma. The main reasons for choosing ERF were fear of infecting the child and work schedule. Only, 38.5% of those who chose ERF made an appropriate choice. However, none of the factors studied was statistically significantly associated to infant feeding choice.
Conclusion: Majority of HIV positive mothers in Bamenda chose EBF over ERF and the main reasons for this choice were financial constraints and fear of stigma. Very few mothers who chose ERF made an appropriate feeding choice for their infants.
Keywords: HIV positive; Mothers; Infant feeding; Choices; Cameroon.
Introduction
Approximately 38.4 million people worldwide are living with HIV (Human Immune Deficiency Virus) of which, 2.73 million [2.06-3.47 million] were children aged 0-19 years in a United Nations International Children’s Educational Fund (UNICEF) reports of 2021 [1]. In Cameroon, about 4300 children were newly infected with HIV in 2021 according to United Nation Program of HIV/AIDS (UNAIDS) [2].Of all these new pediatric infections, more than 90% are as a result of Mother to Child Transmission (MTCT) [2]. Globally, an estimated 1.3 million women and girls living with HIV become pregnant each year [3]. In the absence of any interventions, the rate of transmission of HIV from mother to child during pregnancy, labor, delivery or breast-feeding ranges from 15 to 45% [3].
Infant feeding in the context of HIV is complex because of the major consequences that feeding practices exert on child survival [4]. The dilemma in developing countries is to balance the risk of infants acquiring HIV through breast milk versus other problems of nutrition other than HIV such as diarrhea and malnutrition related to replacement feeding [4]. Hence, prioritization of prevention of HIV transmission needs to be balanced with meeting the nutritional requirements and protection of infants against non-HIV related morbidity and mortality [5]. Feeding of HIV Exposed Infants (HEI’s) poses a major challenge as breastfeeding or poor practices increase transmission of HIV from mother to child, hence impedes the control of spread of HIV/ AIDS [6]. According to WHO, if effective interventions are implemented to Prevent Mother to Child Transmission (PMTCT), the rate can be reduced to less than 5% [6]. In Cameroon, the 2019 national directives for the management of HIV recommend that the option B+ should be used for the PMTCT which is, children exposed to HIV should either receive Exclusive Breast-Feeding (EBF) protected by the administration of oral nevirapine to the child for 6 weeks or Exclusive Replacement Feeding (ERF) till 6 months if living conditions of the mother permits [7].
Irrespective of the feeding choice made by the mothers, when adequately adhered to results in optimal growth and development but unfortunately those who choose ERF in our context and other resource limited countries may not fulfill all the AFASS (Acceptable, Feasible, Affordable, Sustainable, Safe) criteria. This study was aimed at assessing the infant feeding choices, the appropriateness, and the factors influencing the choices made by HIV- positive mothers for their neonates in four hospitals in the Bamenda health district in the North West region of Cameroon.
Materials and methods
The study was a cross sectional analytic study which was conducted in four hospitals in Bamenda, (Regional Hospital Bamenda, Nkwen Baptist Hospital Bamenda, Nkwen District Hospital Bamenda and St. Blaise Catholic Hospital) which is the headquarter of the North-West Region, Cameroon. These four hospitals were selected because they each have over 100 deliveries per month and manage women living with HIV following the National guidelines on the prevention of MTCT of HIV. This study ran from the 14th of February 2023 to 30th of June 2023, and included 166 participants. We included HIV positive postpartum mothers hospitalized in the maternity of the aforementioned hospitals. Sample size was calculated using the prevalence of HIV amongst pregnant women in Cameroon of 2019 which was 4.3% with a confidence interval of 95% and marginal error of 5% giving us a sample size of 63 participants. Data was analyzed with respect to objectives using R software version 4.2.3 and CS Pro version 7.7. We presented results as mean with standard deviation for continuous variables while categorical variables were expressed as proportions or percentages. Statistical significance was defined by a p-value <0.05 using logistic regression analysis to assess association between dependent and independent variables.
During antenatal care, pregnant women received the counseling and testing service and all HIV positive pregnant women were initiated on lifelong combined Anti-Retroviral Therapy (cART) regardless of their immunologic status. During ANC they are provided counseling about PMTCT including infant feeding options which include Exclusive Breast-Feeding (EBF) protected by oral administration of nevirapine to the child for 6 weeks or Exclusive Replacement Feeding (ERF) till 6 months.
Ethical clearance was obtained from the Institutional Review Board of the Faculty of Health sciences, University of Bamenda and administrative authorizations were obtained from the Directors of the study sites. The HIV positive mothers were identified in the post-natal wards of the aforementioned hospitals. Once identified, these women were approached and informed about the study using an information form. Those who met the inclusion criteria and agreed to participate were then required to sign an informed consent form after which they were enrolled. Data was collected using a pretested questionnaire. This questionnaire established the socio-demographic status of the participants, their infant feeding choice alongside the reason for the choice, assessed the appropriateness of replacement feeding using the AFASS criteria and helped determine the factors that influenced the feeding choice made. To note that all through the period of the study, we participated in the different hospitals in counseling activities of HIV positive mothers on feeding options for their neonates at the ANC units.
Results
Socio-demographic characteristics of the mothers
Of 168 HIV positive mothers identified and approached during the study period, 2 refused consent to participate in the study and so a total of 166 HIV positive mothers from the four hospitals were enrolled in the study; 72 from the Regional Hospital Bamenda, 42 From Nkwen Baptist Hospital, 35 from Nkwen District Hospital and 17 from St. Blaise Catholic Hospital. Of these, 127(76.5%) were from an urban area and the rest from rural areas. The age of the mothers ranged from 17 to 44 years with the mean age being 30.6±6.1 years. A majority, 107(64.5%) of the mothers were living as a couple, 62(37.3%) of the mothers and 56(33.7%) of their spouses had attained a primary level of education. Majority, 90(54.2%) mothers and 114(68.7%) spouses had liberal professions. Most, 57(82.5%) of the parents had a lower socio-economic class (Table 1).
Table 1: Socio-demographic characteristics of the study participants.
| Variables | Frequency (n) | Percentage (%) |
|---|---|---|
| Maternal age (years) | ||
| <20 | 3 | 1.8 |
| 20-30 | 71 | 42.8 |
| 30-40 | 79 | 47.6 |
| ≥40 | 13 | 7.8 |
| Mother’s occupation | ||
| Non-Liberala | 13 | 7.8 |
| Liberalb | 90 | 54.2 |
| Unemployed | 63 | 38.0 |
| Mother’s level of education | ||
| No formal education | 16 | 9.6 |
| Primary | 62 | 37.3 |
| Secondary | 55 | 33.1 |
| Higher | 33 | 19.9 |
| Civil status | ||
| Single | 59 | 35.5 |
| Living as a couple | 107 | 64.5 |
| Residence | ||
| Urban | 127 | 76.5 |
| Rural | 39 | 23.5 |
| Spouse’s occupation | ||
| Non-liberal | 23 | 13.9 |
| Liberal | 114 | 68.7 |
| Unemployed | 29 | 17.5 |
| Spouse’s level of education | ||
| No formal education | 21 | 12.7 |
| Primary | 56 | 33.7 |
| Secondary | 51 | 30.7 |
| Higher | 38 | 22.9 |
| Socio economic class | ||
| Upper class | 26 | 15.7 |
| Middle class | 53 | 31.9 |
| Lower class | 87 | 52.4 |
a: with a regular monthly salary; b: with a non- regular monthly salary
Out of the 166 women who participated in our study, 153 of the women practiced exclusive breast-feeding with a prevalence of 92.2% compared to exclusive replacement feeding which was 7.8% (Figure 1). Three main reasons given by the participants for choosing EBF were financial constraint (71.2%), fear of stigma (69.3%), followed by the need for mother-to-child bond (26.8%). Other reasons which some of the women cited were that breast milk contained antibodies and nutrients which will ensure appropriate growth of their infants while others said breast-feeding was less stressful (Figure 2).
Most of the participants (84.6%) who chose ERF gave fear of infecting the infant as reason. A smaller proportion of participants gave as reason because of illness. Other mothers said it was due to their high viral load in pregnancy hence were asked by the health personnel to choose ERF (Figure 3). Out of the 13 participants who practiced exclusive replacement feeding, based on the AFASS criteria, only 5(38.5%) of them made an appropriate choice. The most fulfilled criteria were safe, sustainable and acceptable (Figure 4).
A majority 140(84.3%) of the mother’s HIV status were diagnosed before pregnancy and more than 71.1% of them had disclosed their status to their partners. Half, 83(50%), of their spouses had a negative HIV status. Most (62.7%) of the women were multiparous. The mean number of Antenatal Consultations (ANC) was 6.30±2.1 ranging from 2 to 10 number of ANCs. Majority (52.4%) of the mothers did their ANC in the first trimester with the mean time of first ANC being 14.8±5.3 weeks. All the mothers received counseling on infant feeding choice. Majority 138(83.1%), of them received this counseling during pregnancy and 141(84.9%) of them counseled were counseled by a nurse. Most of these women, 62.7% had a vaginal delivery. None of the factors studied were significantly associated to infant feeding choice (Table 2)
Table 2: Factors associated to infant feeding choice.
| Variables | Infant feeding choice | Odd’s ratio (CI at 95%) | P-value | |
|---|---|---|---|---|
| EBF n(%) | ERF n(%) | |||
| Parity | ||||
| Primipara | 58 (93.5) | 4(6.5) | 1.4 (0.4-4.7) | 0.769 |
| Multipara | 95 (91.3) | 9(8.7) | Reference | / |
| Place of ANC | ||||
| Hospital | 77(91.7) | 7(8.3) | 0.9 (0.3-2.7) | 0.807 |
| Health center | 76 (92.7) | 6(7.3) | Reference | |
| Time of ANC | ||||
| First trimester | 73 (92.4) | 6(7.6) | 1.1 (0.3-3.3) | 0.914 |
| After first trimester | 80 (92.0) | 7(8.0) | Reference | / |
| Number of ANCs done | ||||
| <8 | 86 (92.5) | 7(7.5) | 1.1 (0.4-3.4) | 0.869 |
| ≥8 | 67 (91.8) | 6(8.2) | Reference | / |
| Mode of delivery | ||||
| Per vaginal | 96 (92.3) | 8(7.7) | 1.1 (0.3-3.4) | 1 |
| Caesarean section | 57 (91.9) | 5(8.1) | Reference | / |
| Time of diagnosis of mother’s HIV status | ||||
| Before pregnancy | 130(92.9) | 10(7.1) | Reference | / |
| During pregnancy | 22(88) | 3(12.0) | 1.8(0.5-6.9) | 0.412 |
| Peripartum period | 1(100) | 0(0.0) | / | / |
| Disclosure of status to partner | ||||
| Yes | 110(93.2) | 8(6.8) | 1.6(0.5-5.2) | 0.525 |
| No | 43(89.6) | 5(10.4) | Reference | / |
| Counselling on infant feeding choice | ||||
| Yes | 153(92.2) | 13(7.8) | / | / |
| No | 0(0.0) | 0(0.0) | / | / |
| Time of counselling | ||||
| During pregnancy | 128(92.8) | 10(7.2) | Reference | / |
| After delivery | 13(86.7) | 2(13.3) | 1.9(0.4-9.9) | 0.413 |
| During previous pregnancy | 12(92.3) | 1(7.7) | 1.1(0.1-91) | 0.953 |
| Person who did the counseling | ||||
| Medical doctor | 21(84.0) | 4(16.0) | 0.4(0.1-1.3) | 0.111 |
| Nurse | 132(93.6) | 9(6.4) | Reference | / |
Discussion
Majority of our study population (92.2%) chose exclusive breast-feeding. Higher rates have been observed in some studies [5,6,8,13-18]; These differences might be attributed to differences in knowledge on feeding practices, willingness to practice EBF and different cultural settings.
Lower rates of EBF was observed in some studies [19-21]. This low prevalence compared with our study could be as a result of the difference in study design and study periods. These discrepancies could be due to differences in financial potentials, socio-economic and cultural influence, level of health facility as well as differences in guidelines and recommendations.
The main reasons for choosing EBF in our study were; financial difficulties (71.2%) and fear of stigmatization (69.3%) [8] in Cameroon also registered fear of stigmatization and financial difficulties as reasons for practicing exclusive breast-feeding. While, additional reasons like insufficient knowledge in formula milk preparation and advice from family to practice exclusive breast-feeding were also reported [10,14,18,25,26]. Also, reasons like inconvenience in preparation and administration of formula milk, advice from hospital to practice breast-feeding, and loss of special attention from family were found to militate against artificial feeding [7,8].
The prevalence of ERF was 7.8% in our study which is similar to 7% [12] in Cameroon. Lower prevalence of ERF were observed in other studies [5,17,22,23]. These discrepancies and low rates of ERF could be explained by poverty rates, cultural beliefs and fear of stigmatization where these studies were conducted. Other studies found higher rates of ERF [8,17]. These differences might be due to socio-economic differences, fluctuation in cost of commercial infant formula milk, cultural differences within and across the boundary, and spouse support after status disclosure by the woman could have enhanced increase in rates of ERF in the aforementioned studies.
The main reasons for ERF choice were, fear of infecting the child (84.6%) and work schedule of the mother (46.2%). Other studies [8,16,18,21,22], also noted that most of the women practiced ERF in order to prevent HIV transmission to their babies. However, there were other reasons like, advice from health workers on the risk involved in breast-feeding the baby, free distribution of formula milk and maintaining physical appearance. When replacement feeding is Affordable, Feasible, Acceptable, Safe, Sustainable (AFASS), it is the best possible choice for HIV-positive mothers because formula milk contains no HIV and as such there is no risk of MTCT of HIV through feeding. However, the problem of cost is still very present among HIV-positive mothers in our context, thereby preventing them from choosing it.
Out of the 13 participants who chose replacement feeding, only 38.5% fulfilled all the AFASS criteria hence making their choice inappropriate. The mother’s choice of replacement feeding was said to be appropriate when she fulfilled all the conditions in each AFASS criteria. Our rate was lower than 58.5% and 51.7% [26,27] found in other studies.
None of the factors studied was associated to infant feeding choice. However, other studies found that marital status and the mean number of ANCs was associated to infant feeding choice and number of ANC visits, place of delivery and income level to be statistically significant[11,27]. Also place of delivery and disclosure of status to spouse was significantly associated to infant feeding [14].Meanwhile, mother’s educational status, attendance of ANC visits and disclosure of status to spouse was also significantly associated to infant feeding choice [20,22,25]. The main limitation was that some mothers were reluctant to discuss anything related to their status for fear of stigma.
Conclusion
Majority of HIV positive women preferred exclusive breastfeeding to exclusive replacement feeding and the main reasons for the feeding choices of HIV positive mothers were financial constraints, fear of infecting the child, presence of stigma and the need of mother to child bond. In the mothers who chose exclusive replacement feeding, only one third made an appropriate choice based on the AFASS criteria. None of the factors studied was significantly associated to infant feeding choice.
Declarations
Conflicts of interest: The authors have no conflicts of interest.
Author contributions: All the authors contributed to the design, interpretation of the data, revised the manuscript critically for important intellectual content, gave final approval of the version to be published, and agreed to be accountable for all aspects of the work.
Funding: This study did not receive any funding from any agency.
References
- UNICEF.HIV Statistics - Global and Regional Trends [Internet]. New York: UNICEF 2022; [cited 2022 Nov 20]. Available from: https://data.unicef.org/topic/hivaids/global-regional-trends.
- UNAIDS. Cameroon statistics [Internet]. Geneva: UNAIDS; 2021 [cited 2022 Dec 1]. Available from: https://www.unaids.org/en/regionscountries/countries/cameroon.
- World Health Organization. Mother-to-child transmission of HIV [Internet]. Geneva: WHO; 2022[cited 2022 Nov 5]. Availablefrom:https://www.who.int/teams/global-hiv-hepatitisand-stis-programmes/hiv/prevention/mother-to-child-transmission-of-hiv.
- World Health Organization, United Nations Children’s Fund (UNICEF). Infant and young child feeding counselling: an integrated course: participant’s manual [Internet]. 2nd ed. Geneva: World Health Organization; United Nation Children’s Fund (UNICEF); 2021 [cited 2022 Nov 21]. Available from: https://apps.who.int/iris/handle/10665/346566.
- Ejara D, Mulualem D, Gebremedhin S. Inappropriate infant feeding practices of HIV-positive mothers attending PMTCT services in Oromia regional state, Ethiopia: a cross-sectional study. Int Breastfeed J. 2018; 13(1): 37.
- Ndubuka J, Ndubuka N, Li Y, Marshall CM, Ehiri J. Knowledge, attitudes and practices regarding infant feeding among HIV-infected pregnant women in Gaborone, Botswana: a cross-sectional survey. BMJ Open. 2013; 3(11): e003749.
- Ministry of Public Heath. National guidelines on HIV care. Cameroon: Ministry of Public Health. 2021; 157
- Muko KN, Tchangwe KG, Ngwa VC, Njoya L. Preventing motherto-child transmission: factors affecting mothers’ choice of feeding — a case study from Cameroon. SAHARA-J J Soc Asp HIVAIDS. 2004; 1(3): 132-8.
- Baza D, Abebe A, Markos M. Infant feeding practices among HIV positive mothers enrolled in selected public health institutions of Wolaita, Ethiopia: facility based multicenter cross-sectional study. PAMJ - One Health. 2022; 7(3): 25.
- Suryavanshi N, Jonnalagadda S, Erande AS, Sastry J, Pisal H et al. Infant Feeding Practices of HIV-Positive Mothers in India. J Nutr. 2003; 133(5): 1326-31.
- Mutawulira I, Nakachwa J, Muharabu L, Wilson WA, Kayina V. Exploring infant feeding practices and associated factors among HIV-positive mothers attending early infant diagnosis clinic in Northern Uganda. Epidemiol Infect. 2022; 150(5): e130.
- Ojong AM, Tangwa A, Kwende T, Lum O. Factors assisting HIV + mothers with better feeding options of their babies around the Buea Municipality, Cameroon. Int Res J Med Biomed. 2016; 1(5): 38-44
- Demilew YM, Tafere TE, Abitew DB. Infant and young child feeding practice among mothers with 0–24 months old children in Slum areas of Bahir Dar City, Ethiopia. Int Breastfeed J. 2017; 12(1): 26.
- Muluye D, Woldeyohannes D, Gizachew M, Tiruneh M. Infant feeding practice and associated factors of HIV positive mothers attending prevention of mother to child transmission and antiretroviral therapy clinics in Gondar Town health institutions, Northwest Ethiopia. BMC Public Health. 2012; 12(1): 240.
- Geleto AM, Ahmed KK, Tesfaye TS. Infant Feeding Practice and Associated Factors among HIV Positive Mothers at Health Institution of Shashemene Town, South Ethiopia. J Fam Reprod Health. 2020; 7(8): 25.
- Andare N, Ochola S, Chege P. Determinants of infant feeding practices among mothers living with HIV attending prevention of mother to child transmission Clinic at Kiambu Level 4 hospital, Kenya: a cross-sectional study. Nutr J. 2019; 18(1): 64.
- Sow A, Halle E. Infant feeding practices among HIV positive mothers in three hospitals in Douala: A cross sectional study. [University of Buea]: Faculty of Medicine and Biomedical Sciences. 2022; p\90.
- Aishat U, Olufunmilayo F, David D, Gidado S. Factors Influencing Infant Feeding Choices of HIV Positive Mothers in Southwestern, Nigeria. Am J Public Health Res.2015; 5(3): 72-9.
- Njom AE, Ekani BB. Trends of early infant feedings practices after counseling in infant born to HIV positive women in Yaoundé, Cameroon. Pan Afr Med J. 2014; 17(2): 13.
- Maru Y, Haidar J. Infant feeding practice of HIV positive mothers and its determinants in selected health institutions of Addis Ababa, Ethiopia. Ethiop J Health Dev. 2010; 23(2).
- Olatona F, Ginigeme O, Roberts A, Amu E. Infant feeding practices in the first six months of life among HIV positive mothers attending Teaching Hospitals in Lagos, Nigeria.Niger J Paediatr. 2013; 41(1): 64.
- Bekere A. Exclusive Breast-feeding Practices of HIV Positive mothers and its Determinants in Selected Health Institution of West Oromia, Ethiopia. J Nutr Food Sci. 2014; 04(06): 8.
- Negash S, Mesfin F, Egata G. Infants and young children feeding practice and associated factors among HIV positive mothers of children 0–23 months in health centers of Gulele sub-city, Addis Ababa, Ethiopia. BMC Res Notes. 2019; 12(1): 66.
- Mohammed A, Shehu AU, Aliyu AA, Zoaka AI. Infant feeding options, practices and determinants of feeding practices among HIV seropositive mothers in Abuja, Nigeria. Niger Med J. 2010; 51(1): 14.
- Dagnew AB, Tewabe T, Birhie A, Birehanu M, Alehegn T, et al. Factors Associated with Compliance with World Health Organization-Recommended Infant-Feeding Practices by Mothers with HIV Infection in Northwest Ethiopia. Curr Ther Res. 2019; 91(5): 39-44.
- Bland RM. Infant feeding counselling for HIV-infected and uninfected women: appropriateness of choice and practice. Bull World Health Organ. 2007; 85(4): 289-96.
- Doherty T, Chopra M, Jackson D, Goga A, Colvin M, et al. Effectiveness of the WHO/UNICEF guidelines on infant feeding for HIV-positive women: results from a prospective cohort study in South Africa. AIDS. 2007; 21(13): 1791-7.