Research Article
Volume 3, Issue 5
Patterns and Determinants of Undernutrition in Pre-School Age Children in the North West Region of Cameroon
Andreas Chiabi1*; Rosine Ngum1; Loveline Lum Niba2; Alex Tatang Mambap1; Samuel Angwafor1; Gloria Ashuntantang1,2
1Department of Clinical Sciences, Faculty of Health Sciences, University of Bamenda, Cameroon.
2Department of Public Health, Faculty of Health Sciences, University of Bamenda, Cameroon.
Corresponding Author :
Andreas Chiabi
Email: andy_chiabi@yahoo.co.uk
Received : Mar 19, 2024 Accepted : May 01, 2024 Published : May 08, 2024 Archived : www.meddiscoveries.org
Citation: Chiabi A, Ngum R, Niba LL, Mambap AT, Angwafor S, et al. Patterns and Determinants of Undernutrition in PreSchool Age Children in the North West Region of Cameroon. Med Discoveries. 2024; 3(5): 1149.
Copyright: © 2024 Chiabi A. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background and aim: Malnutrition is a major public health concern for children under five years. About 45% of deaths among children under five years globally are linked to undernutrition.
The aim of the study was to to evaluate the patterns and determinants of undernutrition in pre-school age children in four Subdivisions in Mezam division of the North west region.
Methods: A cross- sectional study in 22 randomly selected schools in four subdivisions in Mezam division, involving 370 children from ages 2 to 5 years old. Anthropometric data was collected using standard procedures. Data on dietary diversity was assessed using a structured questionnaire. Analysis was done using the Statistical Package for Social Science (SPSS) version 26 and WHO Anthro software. Logistic regression analysis was used to assess the relationship between determinants and nutritional status. A p value of less than 0.005 was set as statistical significance.
Results: The mean age of the children was 3.79(±0.84) years and had a female predominance (51.6%). The overall prevalence of undernutrition was 10.8% for which underweight was 1.4%, wasting 1.6%, and stunting 7.8%. The dietary diversity score was low at 65.9%. The most consumed food group was starchy staples, and the least frequently being other fruits and vegetables. Fathers with no formal education (aOR=22.22; 95% CI=0.07-457.79; p=0.045), being an internally displaced child (aOR=7.98; 95% CI=1.45-43.85; p=0.017), and child’s age greater than 3 (aOR=6.42; 95% CI=1.87-22.02; P=0.003) were associated with undernutrition.
Conclusion: Low dietary diversity score, being a father with no formal education, being internally displaced, and the child’s age greater than three years were significantly associated with undernutrition.
Keywords: Nutritional status; Pre-school children; Cameroon; Patterns; Determinants.
Introduction
Malnutrition is a major public concern for children under 5 years. Malnutrition is defined as deficiencies, excesses, or imbalances in a person’s intake of energy and or nutrients [1]. Globally in 2020 it was estimated that 1.9 billion adults were overweight or obese, while 462 million were underweight, 149 million children under 5 were stunted, 45million were wasted and 38.9 million were obese [1]. The Demographic and Health Survey (DHS) in Cameroon in 2004 estimated that 32% of under 5 children were stunted, 18% underweight an 5% wasted [2]. About 45 percent deaths among children under 5 years of age are linked to undernutrition. These mostly occur in low and middle-income countries. The developmental, economic and medical impacts of the global burden of malnutrition are serious and lasting for individuals and their families, for communities and for countries [1].
The etiologies of malnutrition are multifactorial. This include immediate level causes (inadequate dietary intake, underlying disease conditions), Underlying-level causes include insufficient household food security, insufficient health services, and basic level causes, being insufficient resources, sociocultural and political context [3,4].
Malnutrition affects mostly children under five years [5,6]. Death due to common childhood illness is common in malnourished children than with nourished children. Young malnourished children have a compromised immune system which fail to resist infections and are prone to cognitive development delays, long term intellectual deficits as well as physical and mental development [7,8].
Methods
Study setting
The North West region of Cameroon is administratively divided into 7 Divisions, each made up of different subdivisions. The study was conducted in four subdivisions in Mezam Division (Bamenda I, Bamenda II, Bamenda III and Tubah Subdivisions). Mezam is a division of the North West Region of Cameroon made up of 7 Sub Divisions namely: Bamenda I, Bamenda II, Bamenda III, Santa, Tubah, Bafut and Bali. Bamenda doubles as the administrative headquarters of Mezam division and for the North West Region of Cameroon. It is a cosmopolitan city made up of three towns: Mankon, Nkwen and Bamendankwen, inhabited by people from all over the country and neighbouring countries. The population consist of people in the middleincome range with their source of income being mostly business and farming activities. Mezam Division is located in a semi urban and urban area, within which are distributed many public and private nursery schools.
Study design
This was a cross sectional study that was conducted over a period of 5 months, from the 7th of January to the 9th of May 2023.
Data collection
After obtaining ethical clearance from the Institutional Review Board of the Faculty of Health Sciences of The University of Bamenda and Administrative authorization from the Dean of the Faculty of Health Sciences, Regional delegation of public health and Regional delegation of Basic Education North West Region, we proceeded with our study.
The study was detailly explained to the teachers in different schools after presenting an authorization from the Regional Delegate of Basic education. A consent form was given to the parents/care givers in schools to obtain informed and signed consent. Thereafter, data were collected in schools only from pupils whom the parents had accepted to participate in the study.
Anthropometric parameters height, weight, Mid upper arm circumference were collected following standard procedures. Sociodemographic data and data on dietary diversity score was assessed using a structured questionnaire.
Data management and analysis
Data collected was coded and entered into excel sheet and later exported and analysed using Statistical Package for Social Science version 26 (SPSS) and WHO Anthro software. Continues variables were expressed as mean and Standard Deviation (SD), while categorical variables were expressed as percentages or proportions. Statistical significance was defined by a p-value < 0.05 using logistic analysis to assess cause to effect between the independent and dependent variables. Anthropometric indices height/age, weight/height, weight/age, and MUAC were computed and calculated using the WHO anthro software and compared with child growth WHO reference standards. The prevalence of undernutrition was calculated as the proportion of children with undernutrition divided by the total number of children retained in the study times a hundred. The Dietary diversity score was assessed by counting the number of food groups the child ate in the past 24 hours, and classified as low (≤3), Medium (4-5), High (≥6). Associated factors were analyzed by regression analysis (bivariate and multivariate logistic regression).
Results
Worked in 22 nursery schools in four Subdivisions in Mezam Division, approached a total of 510 children out of which 370 were retained and analyzed.
Socio-demographic characteristics of the study population
Children’s age ranged from 2 to 5 years with a mean age of 3.79±0.84, majority aged greater than 3 years 230(62.2%), of female gender 191(51.6%), not internally displaced 316(85.4%) and resident in Urban areas 293(79.2%).
Maternal age ranged from 17 to 64 years with a mean age of 31.13±6.2years, majority of them living as a couple 275(74.3%), aged between 21 to 30 203(54.9%) with household size.
4-10 321(86.8%), had attended the university 157(42.4%), and with liberal occupations 172(46.6%)
Paternal age ranged from 25 to 50years with a mean age of 35.65±4.95, with majority aged between 30 to 40 190(69.1%) and having liberal jobs 183(49.5%). Most parents had a lower socioeconomic status 139(37.6%).
Prevalence of undernutrition
Out of the 370 participants in our study, 40 (10.8) had at least one of the nutritional indices (W/A, W/H, and H/A) less than -2 Z score giving an overall prevalence of 10.8%. This was distributed as follows: W/A 1.4%, W/H 1.6%, and H/A 7.8% (Table 1).
Table 1: Distribution of undernutrition indices.
|
Underweight (W/A<-2 Z score) |
Wasting (W/H&lt;-2 Z score) |
Stunting (H/A&lt;-2 Z score) |
|||
|---|---|---|---|---|---|
| N | % | N | % | N | % |
| 5 | 1.5 | 6 | 1.6 | 29 | 7.8 |
Table 2: Distribution of overnutrition indices.
| Nutritional indices | Number (n) | Percentage (%) |
|---|---|---|
| Overweight (W/H>+2 Z score) | 29 | 7.8 |
| Obesity (W/H>+3 Z score) | 5 | 1.4 |
Similarly, 34(9.2%) children had overnutrition for which 7.8% (29) were overweight and 1.4% (5) obese (Table 2).
Dietary diversity scores of the children.
Majority of children in our study had a low Dietary Diversity Sore (DDS) 9%, with the most consumed food group being starchy staples (Table 3).
Table 3: Dietary diversity scores of the children.
| DDS | Number (n) | Percentage (%) |
|---|---|---|
| Low DDS | 244 | 65.9 |
| Medium DDS | 105 | 28.4 |
| High DDS | 21 | 5.7 |
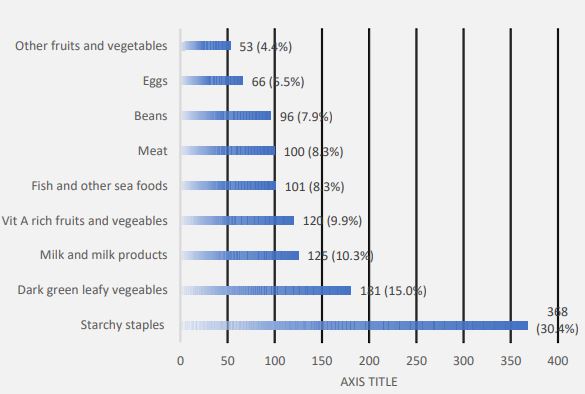
Most of the foods consumed were starchy staple foods (30.4%), leafy vegetables (15%), and milk and milk products (10.3%) (Figure 1).
Table 4: Child’s factors associated with stunting.
| Variable | Z-score <-2 n (%) | Z-score ≥-2 n (%) | OR [95%CI | P- value | Multivariate logistic R aOR [95% CI] | p-value |
|---|---|---|---|---|---|---|
| Age | ||||||
| ≤3 | 3(10.3) | 137(40.2) | Reference | |||
| >3 | 26(89.7) | 204(59.8) | 5.82[1.73-19.61] | 0.004 | 6.42[1.87-22.02] | 0.003 |
| Gender | ||||||
| Female | 14(48.3) | 177(51.9) | Reference | |||
| Male | 15(51.7) | 164(48.1) | 1.16[0.55-2.46] | 0.707 | ||
| Internally displaced | ||||||
| Yes | 3(10.3) | 51(15.0) | 0.66[0.19-2.23 | 0.502 | ||
| No | 26(89.7) | 290(85.0) | Reference | |||
| DDS | ||||||
| Low DDS* | 21(72.4) | 223(65.4) | 1.89[0.25-14.75] | 0.546 | ||
| Medium DDS* | 7(24.1) | 98(28.7) | 1.43[0.16-12.27] | 0.745 | ||
| High DDS* | 1(3.4) | 20(5.9) | Reference | |||
| Residence | ||||||
| Urban | 14(48.3) | 279(81.8) | Reference | |||
| Rural | 15(51.7) | 62(18.2) | 4.82[2.22-10.50] | 0.000 | undefined | |
*dietary diversity score
Table 5: Paternal factors associated with wasting.
| Variables | Z-score <-2 n (%) | Z-score ≥-2 n (%) | OR [95%CI] | p- value | Multivariate logistic R aOR [95%CI] | p-value |
|---|---|---|---|---|---|---|
| Age | ||||||
| [20-30] | 3(50.0) | 49(18.3) | 3.79[0.75-19.39] | 0.109 | ||
| [30-40] | 3(50.0) | 186(69.4) | Reference | |||
| ≥40 | 0(0.0) | 33(12.3) | Undefined | 0.998 | ||
| Level | of | education | ||||
| None | 1(16.7) | 6(1.7) | 19.67[1.09-354.09] | 0.043 | 22.22[1.07-457.79] | 0.045 |
| Primary | 3(50.0) | 98(27.0) | 3.26[0.37-35.28] | 0.269 | 3.98[0.39-39.94] | 0.240 |
| Secondary | 1(16.7) | 47(12.9) | 2.52[0.15-40.98] | 0.518 | 2.07[0.12-35.07] | 0.612 |
| University | 1(16.7) | 118(32.5) | Reference | |||
| Occupation | ||||||
| Liberal | 4(66.7) | 178(49.0) | 0.85[0.15-4.70] | 0.845 | ||
| Non liberal | 2(33.3) | 75(20.7) | Reference | |||
| Unemployed | 0(0.0) | 16(4.4) | Undefined | 0.999 |
Determinants of undernutrition
Child’s factors associated with stunting (HAZ): On bivariate analysis, children greater than 3 years (OR=5.82; CI95(1.73-19..61); p=0.004), and who resided in rural areas (OR=4.82; CI95(2.22-10.50);p=0.000) had higher chances of stunting
On multivariate analysis, the chances of stunting still remained higher in children greater than 3 years (OR=6.42; CI95(1.87-22.02): p= 0.003 (Table 4).
Paternal factors associated with wasting (WHZ): Having a father with no formal education (OR=19.67; CI95(1.09-354.09); p=0.043) was found to increase the chances of wasting.
After adjusting for confounders, the chances of becoming wasted remained higher with a father with no formal education (aOR=22.22; CI95(1.07-457.79); p=0.045) (Table 5).
Factors associated with Wasting (WHZ): As far as factors related to the child are concerned, on bivariate analysis being internally displaced (OR=6.26; CI95(1.23-31.89); P=0.027) increased the chances of wasting
After adjusting for confounders, chances of wasting still remained high by being internally displaced (AOR=7.98; CI95(1.45-43.85); p=0.017) (Table 6).
Table 6: Child’s factors associated with wasting.
| Variable | Z-score <-2 n (%) | Z-score ≥-2 n (%) | OR [95% CI] | p-value | Multivariate logistic R aOR [95%CI] | p-value |
|---|---|---|---|---|---|---|
| Child’s age | ||||||
| ≤3 | 0(0.0) | 140(38.6) | Reference | |||
| >3 | 6(100) | 223(61.4) | Undefined | 0.996 | ||
| Gender | ||||||
| Female | 4(66.7) | 187(51.5) | Reference | |||
| Male | 2(33.3) | 176(48.5) | 0.54[0.09-2.94] | 0.468 | ||
| Internally displaced | ||||||
| Yes | 3(50.0) | 50(13.8) | 6.26[1.23-31.89] | 0.027 | 7.98[1.45-43.85] | 0.017 |
| No | 3(50.0) | 313(86.2) | Reference | |||
| DDS | ||||||
| Low DDS | 5(83.3) | 238(65.6) | Undefined | 0.998 | ||
| Medium DDS | 1(16.7) | 104(28.7) | Undefined | 0.998 | ||
| High DDS | 0(0.0) | 21(5.8) | Reference | |||
| Residence | ||||||
| Urban | 4(66.7) | 288(79.3) | Reference | |||
| Rural | 2(33.3) | 75(20.7) | 1.92[0.35-10.69] | 0.456 |
Discussion
The overall prevalence of undernutrition in this study was 10.8%, with at least one of the weight/age, weight/height, and height/ age less than -2 Z score. Other studies found higher rates, 26.1% in the North region of Cameroon [7], 36.5% in the South West Region of Cameroon [9], and 26.8% in Nigeria [10]. Underweight was observed in 5(1.4%) of children, with none being severely underweight. This measurement reflects both chronic and acute malnutrition. This was lower than the 8.5% observed in North Cameroon [7], the 8.6% in the South West Region of Cameroon [9] and the 10.4% in Ghana [11]. We noted that 7(1.6%) of children were wasted for which 0.5% were severely wasted and 1.1% moderately wasted. The Demographic Health Survey (DHS) in Cameroon [12], noted a prevalence 1.7% of wasting in the North West Region, similar with what we found. Stunting was the most common form of undernutrition with a prevalence of 7.8%, which is far lower than the 26.9% from the Demographic Health Survey in Cameroon [12], 10.3% in North Cameroon [7], 20.9%. in the South West Region of Cameroon [9], and 18.4%. in Ghana [11]. This may be due cultural differences, differences in food supply and the exposure to the different determinants.
Individual dietary diversity scores of the children was low in this study, with a prevalence 65.9%. Low dietary scores were also observed in 75.5% of children in Nigeria [13] and in 73% in Ethiopia [14]. Cereals was the most consumed food group (30.4%) followed by dark green leafy vegetables (14.0%). Low dietary scores reported in this study could be attributed to limited number of food groups, economic reasons and low maternal employment status.
Out of the factors analyzed for underweight, none was found to be statistically significant. Chiabi et al. [7] in a study in North Cameroon in 2011 found a statistically significant relationship between household size and underweight. Njigang et al. [9] in the South west region of Cameroon in 2021 noted household size and maternal marital status to be significantly associated with underweight. We found that children who had fathers with no formal education were likely to be wasted compared to those who had gone to the university. This is similar to the observations by Senthilkumar et al. [15], Islam et al. [16] and Meshram et al. [17] who found that having a father with low level of education increased the chances of wasting. A father with low educational level may not be employed, resulting in poor household finances, food insecurity, and poor general living conditions. Additionally, fathers are more involved in child care by providing financial and physical support to the mother.
Concerning wasting, we also noted that being internally displaced increases the chances of wasting. Internally displaced flee in fear for their lives, abandoning their assets and their social and family network. Majority of them moved from rural to urban areas, a change that has profound humanitarian, economic and social consequences. Economically, displacement results in the loss of assets, capital and labour. These reduce their chances of earning a living and access to basic needs such as adequate food, shelter and health care services which are required for growth. As for stunting, a child being 3 years and above significantly increased the risk of stunting.
This finding is similar to other previous studies in Ethiopia [6], in Ghana [11], and in Nigeria [10] in Nigeria 2014, which observed that older children were more likely to be stunted as compared to younger ones. This is contrary to the findings of Das et al. [18] in India who noted higher rates of stunting in younger children.
As concerns overnutrition, 9.2% of the children had overnutrition. The prevalence of overweight in our study was 7.8% , which was higher than the 6.3% by Tchoubi et al. [19] in Cameroon and 8.8% by Rysha et al [20] in Kosovo. Obesity had a lower prevalence 1.4%, similar to the 1.7% observed by Tchoubi et al. [19], and higher than the 0.5% observed by Chiabi et al. [7]. This study has permitted us to assess and know the nutritional status in this part of Cameroon which has been crisis stricken since 2016. Under and over nutrition are prevalent. Public health interventions on the modifiable determinants will be necessary to alleviate the burden of these nutritional disorders which affect primarily under-fives.
Acknowledgments: Our profound gratitude goes to, the North West Regional delegate of basic education Mr. Ndong Wilfred for his authorization to carry out this work. Sincere thanks to the teachers of the schools selected, the parents and children who accepted to participate in this study and for their cooperation in collecting the data.
References
- WHO Fact sheets – Malnutrition [Internet]. Geneva: WHO; June 2021 [Cited2022Nov 19]. Available from: https://www.who.int/news-room/fact-sheets/detail/malnutrition.
- Institute National de la Statistique (INS) et ORC macro 2004. Enquête Démographique et de sante du Cameroun 2004. Calverton Maryland, USA: INS et ORC macro.
- Laelago Ersado T. Causes of Malnutrition [Internet]. Intech Open; 2022[Cited 2022 Nov 20] Available from: https://doi.org/10.5772/intechopen.104458
- Khan A, Khan S, Zia-ul-Islam S, Tauqeer AM, Riffat, et al. Causes, sign and symptoms of malnutrition among the children. J Nutr Hum Health. 2017; 1(1): 24–7.
- Amosu AM, Degun AM, Atulomah NOS, Olanrewju MA Study of the Nutritional Status of Under-5 Children of Low-Income Earners in a South-Western Nigerian Community. Curr Res.J.Bio. 2011 Sci. 3(6): 578-85.
- Amare ZY, Ahmed ME, Mehari AB. Determinants of nutritional status among children under age 5 in Ethiopia: further analysis of the 2016 Ethiopia demographic and health survey. Glob Health. 2019; 15(1): 62.
- Chiabi A, Nem D, Kobela M, Mbuagbaw L, Ekoe T. Anthropometric measurements of preschool children in North Cameroon. East J Med. 2011; 8.
- Dukhi N. Global Prevalence of Malnutrition: Evidence from literature[Internet]. IntechOpen;2020[Cited 2022 Nov 20]. Available from: https:www.IntechOpen //doi.org/10.5772/92006.
- Agbor Evon Njigang, Sumbele I, Nkweleko Fankam F, Kah E, Ndip RN. Prevalence and risk factors of malnutrition in children zerofive years in Tole Health Area, South West Region of Cameroon. Am J Public Health Res. 2021; 9(2): 71–80.
- Akubugwo EI, Okafor IN., Ezebuo FC. Nutritional status of preschool aged children in Anambra State, Nigeria. IOSR J Pharm Biol Sci. 2014; 9(2): 01-08.
- Boah M, Azupogo F, Amporfro DA, Abada LA. The epidemiology of undernutrition and its determinants in children under five years in Ghana. PLos One. 2019; 14(7): e0219665.
- Institut National de la Statistique (INS). 2021.Enquete Demographique et de sante du Cameroon 2018. Yaounde, Cameroon, Rockville, Maryland, USA;INS et ICF.
- Ogechi UP, Chilezie OV. Assessment of dietary diversity score, Nutritional status and socio-demographic characteristics of under-5 children in some rural areas of Imo State, Nigeria. Mal J Nutr. 2017; 23(3): 425-435.
- Dangura D, Gebremedhin S. Dietary diversity and associated factors among children 6-23 months of age in Gorche district, Southern Ethiopia: Cross-sectional study. BMC Pediatr. 2017; 17: 6.
- Senthilkumar SK, Chacko TV, Suvetha K. Nutritional status assessment of children aged 0-5 years and its determinants in a tribal community of Coimbatore district. Int J Community Med Public Health. 2018; 5: 2835.
- Islam MM, Alam M, Tariquzaman M, Kabir MA, Pervin R, et al. Begum M. Predictors of the number of under-five malnourished children in Bangladesh: application of the generalized poisson regression model. BMC Public Health. 2013; 13: 11.
- Meshram II, Mbbs NA, Balakrishna N, Rao KM, Mbbs AL. Trends in the prevalence of undernutrition, nutrient & food intake and predictors of undernutrition among under five year tribal children in India. Asia Pac J Clin Nutr. 2012; 21: 568-576.
- Das S, Prakash J, Krishna C, Iyengar K, Venkatesh P. Assessment of nutritional status of children between 6 months and 6 years of age in Anganwadi centers of an urban area in Tumkur, Karnataka, India. Indian J Community Med. 2020; 45(4): 482.
- Tchoubi S, Sobngwi-Tambekou J, Noubiap JJN, Asangbeh SL, Nkoum BA, et al. Prevalence and Risk Factors of Overweight and Obesity among Children Aged 6–59 Months in Cameroon: A Multistage, Stratified Cluster Sampling Nationwide Survey. PLOS One. 2015; 10(12): e0143215.
- Rysha A, Gjergji TM, Ploeger. Nutritional status of preschool children attending kindergartens in Kosovo. J Health Popul Nutr. 2017; 36(1): 26.