Short Report
Volume 3, Issue 4
High Intercostal Space Twelve-Lead ECG in Arrhythmogenic Cardiomyopathy
Stefan Peters*
Internal Department and Cardiology, Ubbo Emmius Hospital Norden, Germany.
Corresponding Author :
Stefan Peters
Tel: +49-4931-181-435;
Email: h.u.s.peters@t-online.de
Received : Mar 02, 2024 Accepted : Apr 10, 2024 Published : Apr 17, 2024 Archived : www.meddiscoveries.org
Citation: Peters S. Typical Electrocardiographic Features in Arrhythmogenic Left Ventricular Cardiomyopathy. Med Discoveries. 2024; 3(4): 1143.
Copyright: © 2024 Peters S. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
The value of high intercostal spaces of lead V1 and V2 is analyzed in arrhythmogenic cardiomyopathy. In this ECG writing technique a localized right precorial QRS prolongation and right precordial T-wave inversion can be demonstrated. In normal intercostal spaces only electroanatomic scar and myocardial atrophy documented in lead aVR was present.
Keywords: Brugada syndrome; Arrhythmogenic cardiomyopathy; High intercostal space; Right precordial T-wave inversion; Localized right precordial QRS prolongation.
Introduction
An expert consensus statement in 2014 assessed the value of high intercostal spaces in Brugada syndrome [1]. The exact anatomical location of the right ventricular outflow tract was assessed by echocardiography.
Little is known using the same technique in arrhythmogenic cardiomyopathy by multichannel electrocardiogram diagnostics [2]. In cases of non-diagnostic criteria higher intercostal spaces could belong to a technical improvement, as ECG criteria belong in most cases to a positive approach in diagnostic criteria.
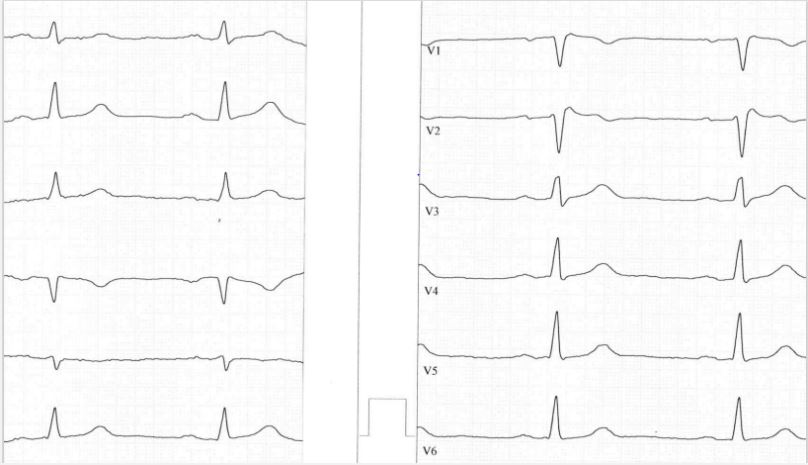
By routine approach the ECG of a 52-year old female patient was assessed from the psychologic department. The patient suffered from endogenic depression. Incidentically, the ECG was written at high intercostal spaces of lead V1 and V2. An rSr‘ complex was documented in lead V1 and V2 with a Brugada type 2 pattern (Figure 1). The ECG revealed a tremendous localized QRS prolongation in right precordial leads and the phenomenon of T-wave inversion in lead V1 > lead V2. The patient was completely asymptomatic, no palpitations, no runs of heart rush and no syncopes.
In echocardiography the right ventricle was dilated with decreased TAPSE and the dimension of the RVOT and the inferior area of the right ventricle were dilated.
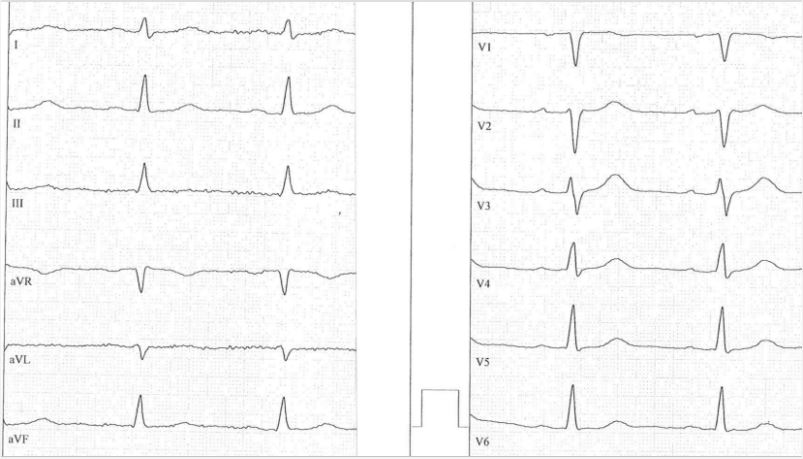
The ECG writing was redone at normal intercostal spaces and revealed a distinct localized prolongation of the QRS complex in right precordial leads, no right precordial T-wave inversions and no signs of right precordial epsilon waves. In lead aVR a large Q wave, a small R wave and negative T waves were present (Figure 2).
In conclusion, ECG writing at hight intercostal spaces of lead V1 and lead V2 enhances typical ECG features of arrhythmogenic cardiomyopathy demonstrating localized right precordial QRS prolongation [3] and terminal activation delay [4], right precordial T-wave inversions and the phenomenon of T-wave inversion in lead V1 > lead V2, possible epsilon wave in lead V2 [5], and typical findings in lead aVR representing electroanatomic scar and myocardial atrophy [6].
A typical pattern of Brugada syndrome could be excluded by documentation of a rSr‘ pattern in lead V1 and lead V2 with a Brugada type 2 pattern [7].
In cases of non-conclusive ECG criteria a ECG technique with higher intercostal spaces - as applied in Brugada syndrome as a recommended approach - could be a valuable approach also in arrhythmogenic cardiomyopathy. In few cardiological departments used a multichannel ECG approach, but using higher intercostal spaces only in lead V1 and lead V2 is a simple approach applicable in every ECG laboratory.
Limitations: As this is a single description of an incidental case more data would be analyzed in higher intercostal spaces of lead V1 and V2 in a representive study in probable cases of arrhythmogenic cardiomyopathy to draw a better conclusion of the value of the special ECG writing technique.
References
- Savastano S, Rordorf R, Vicentini A, Petracci B, Tarvelli E, et al. A comprehensive electrocardiographic, molecula, and echocardiographic study of Brugada syndrome: Validation of the 2013 diagnostic criteria. Heart Rhythm. 2014; 11: 1176-83.
- Marcinkevics R, O’Neill J, Law H, Pervolaraki E, Hogarth A, et al. Multichannel electrocardiogram diagnostics for the diagnosis of arrhythmogenic right ventricular dysplasia. Europace. 2018; 20: f13-f19.
- Peters S, Trümmel M, Koehler B, Westermann KU. The value of different electrocardiographic depolarization criteria in the diagnosis of varrhythmogenic right ventricular dysplasia/cardiomyopathy. J Electrocardiol. 2007; 40: 34-7.
- Cox MG, Van den Smagt JJ, Wilde AA, Wiesfeld AC, Atsma DE, et al. New ECG criteria in arrhythmogenic right ventricular dysplasia/cardiomyopathy. Circ Arrhythm Electropysiol. 2009; 2: 524- 30.
- Zhang L, Liu L, Kowey PR, Fontaine GH. The electrocardiogaphic manifestations of arrhythmogenic right ventricular dysplasia. Curr Cardiol Rev. 2014;10: 237-45.
- Peters S. Clinical importance of lead aVR in arrhythmogenic cardiomyopathy. Int J Cardiol. 2014; 176: 508-9.
- Peritz DC, Chung EH. Criteria for evaluating rSr‘ patterns due to high precordial ECG lead placement accurately confirm absence of a Brugada ECG pattern. J Electrocardiol. 2016; 49: 182-6.