Research Article
Volume 3, Issue 3
The Effective Factors on the Adherence to Drugs Treatment Behaviors in Multiple Sclerosis Patients Based on Theory Planned Behavior
Sara Hamtaeigashti1 ; Mohsen Shamsi2*; Mohammad Ali Sahraian3 ; Raheleh Soltani2 ; Amir Almasi-Hashiani4
1Department of Health Education, Student, Research Committee, Faculty of Health, Arak University of Medical Sciences, Arak, Iran.
2Department of Health Education and Health Promotion, Faculty of Health, Arak University of Medical Sciences, Arak, Iran.
3Multiple Sclerosis Research Center, Neuroscience Institute, Tehran University of Medical Sciences, Tehran, Iran.
4Department of Epidemiology, Faculty of Health, Arak University of Medical Sciences, Arak, Iran.
Corresponding Author :
Mohsen Shamsi
Email: Mohsen shamsi1360@yahoo.com & dr.shamsi@arakmu.ac.ir
Received : Feb 22, 2024 Accepted : Mar 11, 2024 Published : Mar 18, 2024 Archived : www.meddiscoveries.org
Citation: Hamtaeigashti S, Shamsi M, Sahraian MA, Soltani R, Almasi-Hashiani A. The Effective Factors on the Adherence to Drugs Treatment Behaviors in Multiple Sclerosis Patients based on Theory Planned Behavior. Med Discoveries. 2024; 3(3): 1129.
Copyright: © 2024 Shamsi M. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objective: In Multiple Sclerosis (MS), non-adherence is related to suboptimal response to treatment, including disease relapses and the need for more expensive healthcare. The aim of this study was to identify predictors related to treatment adherence drugs in Iranian MS patients.
Methods: In this cross-sectional descriptive-analytical study, 269 patients with M.S, who referred to Tehran, Hospital Sina Clinic in 2021-2022, were selected by systematic random sampling method. The data were collected through a researcher-made questionnaire including knowledge, TPB construct, and performance of patients in the field of treatment adherence drugs. The data were analyzed by SPSS 16 software using Pearson correlation coefficient and linear regression analysis.
Results: The mean age at study entry for patients was 35.04±9.63 years, 220(81.8%) were female. The mean scores of knowledg (4.76±1.7), the performance of treatment adherence drugs (3.50±0.42), attitude (3.86±0.45), subjective norm (3.96±0.56), perceived behavior control (3.84±0.57), intention (4.35±0.52) were obtained. The performance treatment adherence drugs were observed never adherence drugs 3% (9 patients), rarely 5% (14 patients), sometimes 10% (26 patients), often 21% (56 patients) and always 61% (164 patients). The overall adherence rates in the study 87% observed. In this study, intention and perceived behavior control were the strongest predictors of treatment adherence drugs that predicted 29% (R2 =0.291, B=0.334, P=0.001) of behavior variance.
Conclusion: According to the results of the study, in designing educational interventions, the construct of perceived behavior control and intention should be considered as the most important predictor of Patients behavior.
Keywords: Multiple sclerosis; Adherence; TPB; Predictive.
Abbreviations: MS: Multiple Sclerosis; TPB: Theory of Planned Behavior; CVR: Content Validity Ratio; CVI: Content Validity Index; SD: Standard Deviation.
Introduction
Multiple Sclerosis (MS) is a chronic neurological disease that affects more than 2.5 million people worldwide. The exact cause of the disease is not known, but it appears that a combination of genetic traits and environmental factors causes an autoimmune disorder in a person’s central nervous system [1,2]. Medication adherence is one of the most important pillars in the treatment of MS patients. Adherence is defined as the active, voluntary, and cooperative participation of the patient that results in the establishment of acceptable behavior to maintain the desired outcome of prevention or treatment [3]. The rate of medication adherence has been reported to range from 49% to 88% in MS patients in various studies [4,6]. In the study by Alonso et al. the rate of medication adherence in MS patients was 79.7% in Argentina and 76% in Ecuador [7]. The definition of adherence based on WHO definition is the extent to which a person’s behavior taking medication, following a diet, and/ or executing lifestyle changes corresponds with agreed recommendations from a health care provider [1]. In the longitudinal study by Mohr et al. there was a direct association between MS patients who were unable to self-inject the drug and discontinuation of the drug during the first six months of treatment [8]. In the study by Dashti et al. emphasizing self-care behaviors in female patients with MS was effective in controlling complications caused by MS [9]. Attempting to maximize adherence to the prescribed treatment regimen is the surest way to better disease control. Patient education is one of the most important aspects to increase medication adherence [10]. In this context, it is useful to draw on theories of health behavior to better understand the factors that influence patient behavior and to ensure more effective education. One of these theories is the Theory of Planned Behavior (TPB) which predicts the occurrence of a certain behavior, provided that the person intends to do it. According to this theory, the intention to perform a behavior is predicted by three factors: attitude toward behavior, subjective norms, and Perceived Behavioral Control (PBC) [11,12]. Armitage showed that PBC, together with intention, explained 27% of the variance in physical activity behavior [13]. Treatment adherence drugs in MS is one of the key factors determining therapeutic success. To date, there are few studies that analyze the factors that influence the degree of adherence to treatment of these patients in our region. For this reason, the objective of our study was to analyze this phenomenon. Considering the importance of medication adherence in MS patients, especially in the context of the COVID-19 pandemic, and the need to investigate the factors that influence patients› behavior, the aim of the present study was to determine the predictive power of the TPB in improving the medication adherence of MS patients, so that on this basis it is possible to increase patients medication adherence and reduce the complications of the disease, while emphasizing the training of these behaviors.
Materials and methods
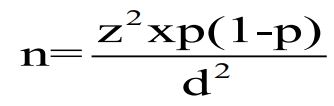
Study design: The present study was analytically conducted on 269 MS patients treated with Disease-Modifying Drugs (DMDs), interferon beta-1a (Rebif), and referred to the Multiple Sclerosis Subspecialty Clinic of Sina Hospital in Tehran, Iran, during 2021-2022. The inclusion criteria were patients with Relapsing-Remitting MS (RRMS) treated with interferon beta-1a (Rebif), patients who lived in Tehran and had a medical record at Sinai Hospital in Tehran, and patients who consented to participate in the study. The sample size was 269 subjects based on the following formula, with 50% patient medication adherence, alpha of 5%, and error in estimating prevalence of 6%.
Sampling was based on the Clinic’s patient list and according to the study’s inclusion criteria using a table of random numbers.
Validity and reliability of questionnaire: The development of the TPB in patients with MS - a questionnaire intended to an explain patient choices to use or not to use treatment adherence drugs was based on the instructions given by Ajzen [28]. We focused on assessing all relevant awareness, cognitive and emotional issues (belief composites) presumably processed by MS-patients considering a performance about treatment adherence drugs. The original pool of about 85 awareness and belief composites was generated by extracting salient statements from interview with 30 physician patient consultations on treatment adherence drugs performance. Statements identified as relevant were classified according to their underlying constructs in terms of the TPB framework. They were allocated to knowledge and one of the three main domains TPB (attitude, subjective norm, and PBC) this pool of knowledge and belief composites and their allocation were discussed and supplemented by an expert panel of three MS and related disorders specialist, two neurology specialist, one general physician, two health education and health promotion specialist, one nurse expert in MS and one specialist in epidemiology. The conceptual framework of the validity and reliability of this study was that according to the similar study Kasper et al. [29] about developing, validity and reliability questionnaire based on TPB. During this process, based on a study Kasper et al. [29] classification of the statements was checked and about 8 new statements were added from nurse and physicians’ clinical practice. In the next step, based on the underlying concept items were created to exhaustively cover the TPB framework for the scenario of performance treatment adherence drugs. With regard to uniqueness, similarity and disjunctiveness, primary instrument were piloted with 15 MS patients in the MS outpatient clinic to check comprehensibility and relevance. The final questionnaire consisted of 47 items including Knowledge, construct of the TPB domains and the performance questionnaire on treatment adherence drugs. The validity and reliability of this questionnaire was approved and it was completed before the training intervention and three month after the intervention by both control and intervention groups. In this tool, those questions with Content Validity Ratio (CVR) score higher than 0.62 and Content Validity Index (CVI) score higher than 0.79 were considered as appropriate and included in the study [22]. To verify its reliability, the questionnaire was given to 30 MS patients and its reliability was calculated as upper 0.8 using Cronbach’s alpha.
Data collection
The questionnaires used in the present study were as follows: Questionnaire on patient demographic characteristics: Age patients, Age of morbidity of MS based on diagnosis date, gender, education, employment status, marital status, economic status, health insurance status, mobility limitations, and how to obtain education.
Questionnaire on the constructs of awareness and TPB: This questionnaire contains 47 questions (measuring awareness=8 questions, theoretical constructs including measuring attitude=8 questions, measuring behavioral intention=4 questions, measuring perceived behavioral control=7 questions, measuring subjective norm=7 questions, and measuring performance=13 questions). The section on awareness, which contained 8 questions, aimed to assess the level of awareness of MS patients regarding MS disease and medication adherence, time to visit a physician, symptoms of an attack, methods of controlling disease symptoms, methods of controlling drug side effects, and methods of controlling injection site side effects. A correct answer received a score of one, an incorrect answer received a score of zero, and the range of awareness scores was from zero to eight. Regarding the TPB constructs, there were five response options: I fully agree, I agree, I have no opinion, I disagree, and I disagree at all, and the range of scores was from one to five. Therefore the scores range of each theory construct was reported between one and 5. The questions of performance treatment adherence drugs questionnaire (for example drug dose, time use, type of drugs, reducing or increasing the amount of medication without prescribe physician, changing the timing of intake, forgetting to take medication and so on) were assessed two week ago and scored on a 5-point scale of behavior evaluation from never, rarely, sometimes, often and always scoring from 0 to 4 and the scores in this part were reported between 0 and 4. According to Ajzen (who is one of the founders of the theory of planned behavior), using the self-report method and relying on individual’s reports rather than direct observation and immediate measurement of the target behavior, due to some problems in obtaining data in the time limits, is an accepted method in TPB studies [26,27]. In this study higher score indicate higher level (considered to be a «good» score) of knowledge, attitude, subjective norms, PBC, intention and performance of treatment adherence drugs in patient with MS.
Data analysis: Data obtained from the questionnaire were analyzed using SPSS [16]. Descriptive statistics were used to describe the characteristics of the study units, and the linear regression test, chi-square test, Pearson correlation coefficient, and t-test were used to evaluate the effect of variables predicting patients’ medication adherence.
Results
The mean age at study entry for patients was 35.04±9.63 years. The mean age of morbidity to MS patients based on diagnosis date was 32.48±9 years 220(81.8%) were female, and the mean treatment adherences drugs score was 3.5±0.42. Most patients were unemployed 154(57.2%) and had a academic education 144(54%). No significant difference was found in the mean performance score related to medication adherence by gender (p=0.129), previous education (p=0.89), marital status (p=0.99), and employment status (p=0.054). Complete baseline aspects of included patients are shown in Table 1. As for the mean and standard deviation of the TPB constructs, this value was found to be 3.86 for the attitude construct with a standard deviation of 0.45. The mean values of the other theoretical constructs are illustrated in Table 2. The mean treatment adherences drugs score was 3.50±0.42. The performance treatment adherence drugs based score on a 5-point scale of behavior evaluation were observed never adherence drugs 3% (9 patients), rarely 5% (14 patients), sometimes 10% (26 patients), often 21% (56 patients) and always 61% (164 patients). In this study 61% of patients had a highest performance treatment adherences (always) and 3% had a lowest adherence drugs (never). The mean scoring treatment adherence drugs or the overall adherence rates in the study 87% observed (between range of 3%-61%). Some of the most common behaviors of medication non adherence observed in patients with medication non-adherence were reducing the amount of medication prescribed (67%), reducing intake due to feeling healthy (58%), reducing intake due to side effects (56%), not taking one dose of medication (51%), not taking multiple doses of medication (46%), changing the timing of intake (42%), taking too much medication (34%), and forgetting to take medication (30%), respectively. Regarding the correlation coefficient of the TPB constructs with the medication adherence of MS patients, the results of the study indicated that the highest correlation was between the construct of attitude and patients’ medication adherence (r=0.167 and p=0.006). Patients awareness had a significant relationship with attitude (r=0.277), PBC (r=0.184), and subjective norms (r=0.207). Performance was significantly related to age (r=0.132), age at onset MS (r=0.119), PBC (r=0.149), and subjective norms (r=0.137). Additional correlation results are displayed in Table 3. Patients most common subjective norms included following recommendations from nurses (87%), physicians (84%), family and friends (77%), educational books and CDs (73%), and recommendations from other MS patients (64%). Regarding the regression analysis of the constructs predicting medication adherence of MS patients, the results demonstrated that the constructs of behavioral intention and PBB as the strongest predictors accounted for a total of 29% of the variance in behavior (Table 4).
Table 1: Formula for MI lozenges.
| Variables | N (%) |
Adherence treatment drugs (Mean±SD) |
P-value | |
|---|---|---|---|---|
| Gender | Female | 220(81.8) | 3.53±0.40 | 0.129* |
| Male | 49(18.2) | 3.40±0.52 | ||
| Marital status | Married | 144(53.5) | 3.52±0.40 | 0.994* |
| Single | 125(46.5) | 3.48±0.41 | ||
| Heath insurance | Yes | 247(91.8) | 3.49±0.42 | 0.135* |
| No | 22(8.2) | 3.64±.40 | ||
| Employ status | Employee | 154(57.2) | 3.55±0.41 | 0.057* |
| Unemployed | 115(42.8) | 3.45±0.43 | ||
|
Educational qualification |
Elementary | 55(20) | 3.41±0.40 | 0.038** |
| Diploma | 70(26) | 3.44±0.35 | ||
| University | 144(54) | 3.59±.040 | ||
| Income level | Weak | 53(19.7) | 3.45±0.46 | 0.008** |
| Medium | 103(38.3) | 3.51±0.42 | ||
| Good | 113(42) | 3.61±0.31 | ||
|
Movement restriction |
Yes | 2(0.7) | 3.5±0.05 | 0.875* |
| No | 267(99.3) | 3.52±0.42 | ||
| Living alone | Yes | 24(8.9) | 3.36±0.51 | 0.013* |
| No | 245(91.1) | 3.54±0.41 | ||
|
Receive previous education |
Yes | 124(46.1) | 3.71±0.37 | 0.021* |
| No | 145(53.9) | 3.32±0.48 | ||
|
How to get training |
Face to face | 164(61) | 3.51±0.42 | 0.279** |
| Educational film | 97(36) | 3.48±0.43 | ||
|
Booklet and pamphlets |
8(3) | 3.62±0.33 |
*T-test
**ANOVA
Table 2: The mean (SD) of TPB construct and frequency of adherence treatment drugs in pa- tients with multiple sclerosis (n=269).
| Construct of TPB | Mean* | SD | Minimum | Maximum | Range of score |
|---|---|---|---|---|---|
| Knowledge | 4.76 | 1.7 | 0 | 8 | 0-8 |
| Attitude | 3.86 | 0.45 | 2.25 | 4.63 | 5-Jan |
| Subjective norm | 3.96 | 0.56 | 2.14 | 5 | 5-Jan |
| Perceived behavior control | 3.84 | 0.57 | 2.43 | 5 | 5-Jan |
| Intention | 4.35 | 0.52 | 2.75 | 5 | 5-Jan |
| Performance | 3.5 | 0.42 | 2.15 | 4 | 0-4 |
| Adherence treatment drugs | Never | Rarely | Sometimes | Often | Always |
| (number of patients and percent) | 9(3%) | 14(5%) | 26(10%) | 56(21%) | 164(61% |
* The higher score Indicate higher level of knowledge, attitude, subjective norms, perceived behavior control, intention and performance of treatment adherence drugs in patient with MS.
Table 3: Correlation between construct of TPB and adherence treatment drugs in patients with multiple sclerosis.
| Variables | Age |
Age of morbidity MS |
Knowledge | Attitude | Intention |
Perceived behavior control |
Subjective norm |
Performance | |
|---|---|---|---|---|---|---|---|---|---|
| Age | Correlation coefficient | 1 | |||||||
| P-value | 0 | ||||||||
| Age of morbidity MS | Correlation coefficient | 0.973 | 1 | ||||||
| P-value | 0.001 | 0 | |||||||
| Knowledge | Correlation coefficient | 0.03 | 0.02 | 1 | |||||
| P-value | 0.967 | 0.743 | 0 | ||||||
| Attitude | Correlation coefficient | 0.136 | 0.098 | 0.277 | 1 | ||||
| P-value | 0.026 | 0.108 | 0.001 | 0 | |||||
| Intention | Correlation coefficient | 0.087 | 0.055 | 0.074 | 0.56 | 1 | |||
| P-value | 0.155 | 0.371 | 0.225 | 0.001 | 0 | ||||
| Perceived behavior control | Correlation coefficient | 0.016 | 0.008 | 0.184 | 0.45 | 0.479 | 1 | ||
| P-value | 0.794 | 0.89 | 0.002 | 0.001 | 0.001 | 0 | |||
| Subjective norm | Correlation coefficient | 0.103 | 0.071 | 0.207 | 0.287 | 0.37 | 0.133 | 1 | |
| P-value | 0.093 | 0.244 | 0.001 | 0.001 | 0.001 | 0.03 | 0 | ||
|
Performance in treatment adherence drugs |
Correlation coefficient | 0.132 | 0.119 | 0.09 | 0.167 | 0.115 | 0.149 | 0.137 | 1 |
| P-value | 0.03 | 0.052 | 0.14 | 0.001 | 0.06 | 0.015 | 0.025 | 0 |
Table 4: Simple linear regression analysis for prediction of treatment adherence drugs in patients with multiple sclerosis (n=269).
| Predictors Variables | Un standardized coefficients | standardized coefficients | t | p | Adjusted R2 |
|---|---|---|---|---|---|
| Intention | 0.293 | 0.317 | 6.4 | 0.001 | 0.291 |
| Perceived behavior control | 0.532 | 0.334 | 6.8 | 0.001 |
Discussion
PBC and behavioral intention predicted 29% of medication adherence in MS patients. Patient medication adherence performance was significantly related to the variables of patient age, attitude, and PBC. In the present study, as patients aged, medication adherence also increased. The reason for this may be that the study was conducted during the COVID-19 pandemic, which resulted in higher medication adherence in elderly patients because of various warnings about the vulnerability of patients with chronic conditions, including MS. Other possible reasons for the correlation between age and medication adherence such as the idea that as people age they take their illnesses more seriously, or as they age they learn more about their disease and are thus more willing to try to intervene through medications. In the current study, the awareness score of MS patients was low in terms of medication adherence, considering the patients’ educational status (more than half of the patients had a university education). This result indicates that patients are not able to properly understand medication adherence based on their educational status alone and that people with high educational status are also prone to medication non adherence. This result is not consistent with the study of Dinesh K Upadhyay et al. on nutritional therapy in diabetic patients [14]. In the present study, one of the reasons for the low level of knowledge of the MS patients regarding the drug regimen could be that the diagnosis of the disease was recent and the patients were not sufficiently informed about the nature of the disease and the drug regimen. The constructs of attitude and subjective norm were directly and significantly related to patients’ medication adherence, making it possible to improve patients’ attitudes and their impact on their behavior through educational programs. In terms of assessing patient attitudes toward future behavioral outcomes, Gerber’s study showed that patients who fully adhered to their medications had lower rates of MS-related hospitalizations and reactions related to their injection than those who did not fully adhere to medications, and that adherence generally reduced many costs [15]. Therefore, emphasizing the construct of attitude in educational programs may be effective to some degree in promoting medication adherence. Moreover, Filipi et al. have suggested that the most common side effects of interferon injections, which include cold-like symptoms and allergic reactions at the injection site, can be managed by educating MS patients [16]. Other studies have reported that patient education and support have a positive impact on patient medication adherence [17,18]. According to the results of the present study, most of the patients’ subjective norms were related to the treatment staff, including nurses and physicians, who were the motivating source for patients to adhere to the medication. The study by Burke et al. on subjective norms highlighted the effective role of nurses in MS patient medication adherence [19]. In addition, Zimmer et al. rated nurses’ education as more effective than physicians’ education on medication adherence in MS patients [20]. Considering the direct relationship between PBC and patients’ medication adherence, it is reasonable to assume that this construct could have a major impact on behavior change [21,22,29]. In this study, the constructs of PBC and behavioral intention were found to be as predictors of patients’ medication adherence at a rate of 29%. Since these two constructs can have a strong relationship with the occurrence of a behavior, they are in fact the entry point to the performance of a behavior that should be taken into account, because just knowing what a person should do and knowing the causes of that behavior is not enough for him, but he must consider himself capable of performing that particular behavior. Studies have shown that perceived competence has a strong impact on patients’ health behaviors, increasing their ability, skill, competence, and appropriateness [23,24] in this study 61% of patients had a highest performance treatment adherences (always) and 3% had a lowest adherence drugs (never) and the overall adherence rates in the study 87% observed. Infact in the current study, the performance of patients in taking medication adherence was higher than the average, with considering patients who referred to clinic, were selected by systematic random sampling method the reason for this could be the simultaneous conduct of the study in the conditions of the COVID-19 pandemic and the impact of media advertising on patients’ susceptibility and their greater importance to their health, resulting in the improvement in medication adherence. However, the reasons for medication non-adherence, e.g. reducing the amount prescribed or taking medications when one feels healthy, demonstrate the need for education. The rate of medication adherence has been reported to range from 49% to 88% in MS patients in various studies [4,6]. The rate of medication adherence in MS patients was 79.7% in Argentina and 76% in Ecuador [7]. Dhib Jalbut et al. in their intervention study expressed that nursing support along with reducing the side effects of drugs at baseline had a significant effect on increasing patient medication adherence [25].
One of the limitations of the study was the condition of the COVID-19 pandemic, leading to the lower number of visits of patients to the MS clinic, which increased the sampling time in this study. Finally, in this study we are using a self-reported Questionnaires. This limitation was resolved by allocating sufficient time and explicit expression of the objectives of study, and gathering information along with interviewing. It is suggested that the medication adherence behavior of MS patients should be studied on the basis of other behavioral theories and the effective constructs of controlled educational experiments on these patients. In future studies in addition to the questionnaire, clinical tests and examinations for MS patients are also used to assess outcome of health behaviors and treatment adherence drugs.
Conclusion
To improve patient medication adherence in educational programs, emphasizing the construct of PBC to empower patients, improve attitudes and understanding of the consequences of medication non-adherence by creating behavioral intentions, can be effective in increasing patient medication adherence. The results of this study can be used to provide appropriate information on the causes of medication non-adherence and to empower patients in the areas of drug injection, overcoming injection phobia, and providing information and awareness about the nature of the disease and proper understanding of the drug regimen to reduce the complications of the disease.
Declarations
Acknowledgment: We would like to thank all of the patients who participated in this study.
Authors’ contribution statements
Conceptualization: Mohsen Shamsi, Mohammad Ali Sahraian, Raheleh Soltani.
Data curation: Sara Hamtaeigashti, Amir Almasi-Hashiani.
Formal analysis: Amir Almasi-Hashiani.
Funding acquisition: Mohsen Shamsi.
Investigation: Sara Hamtaeigashti.
Methodology: Mohsen Shamsi, Mohammad Ali Sahraian, Raheleh Soltani, Amir Almasi-Hashiani.
Project administration: Mohsen Shamsi.
Resources: Mohsen Shamsi, Mohammad Ali Sahraian, Raheleh Soltani.
Supervision: Mahmood Karimy.
Validation: Mohsen Shamsi, Mohammad Ali Sahraian, Raheleh Soltani.
Visualization: Mohsen Shamsi, Mohammad Ali Sahraian, Raheleh Soltani.
Writing original draft: Sara Hamtaeigashti, Mohsen Shamsi, Mohammad Ali Sahraian, Raheleh Soltani.
Writing review and editing: Mohsen Shamsi, Mohammad Ali Sahraian, Raheleh Soltani.
Conlicts of interest/compeing interests: The authors declare that they have no conflict of interests.
Ethical approval: The present study was approved by Research Council of Arak University of Medical Sciences (Grant Number: 6425). The ethics committee approval code number is (IR.ARAKMU.REC. 1400.82).
Consent to participate: Informed written consent was obtained from the patients and all the procedures performed in the study involving human participants, were in accordance with the ethical standards.
Funding: The present study is taken from a master thesis approved by Arak University of Medical Sciences (Grant Number:6425). The funder provided all costs of the thesis and has not any role in the conducting and report of the study results.
References
- World Health Organization. Adherence to Long-Term Therapies: Evidence for Action. Geneva: WHO. 2003.
- Halpern R, Agarwal S, Dembek C. Comparison of adherence and persistence among multiple sclerosis patients treated with disease-modifying therapies: a retrospective administrative claims analysis. Patient Prefer Adherence. 2011; 5: 73-84.
- Namey MA. Promoting adherence to complex protocols. Advanced concepts in multiple sclerosis nursing care. 2007; 91: 100.
- Ben-Zacharia A, Adamson M, Boyd A. Impact of shared decision making on multiple sclerosis. Int J MS Care 2018; 6: 287-297.
- Kołtuniuk A and Rosińczuk J. Adherence to disease-modifying therapies in patients with multiple sclerosis. Patient Prefer Adherence. 2018; 12: 1557-1566.
- Zanga G, Drzewiscki E, Tagliani P, Smietniansky M, Maria M, Rojas E, et al. Predictors of adherence and persistence to diseasemodifying therapies in Multiple Sclerosis. Therapeutic Advances in Neurological Disorders. 2021; (14): 1-11.
- Alonso R, Rojas J, Ramos J, Correa P, Pita C, Cohen S. et al. Evaluation of adherence to treatment in patients with multiple sclerosis from Latin America. Multiple Sclerosis and Related Disorders. 2022; (63): 1039-15. https://doi.org/10.1016/j.msard.2022.103915 Get rights and content.
- Mohr DC, Boudewyn AC, Likosky W, Levine E, Goodkin DE. Injectable medication for the treatment of multiple sclerosis: the influence of self-efficacy expectations and infection anxiety on adherence and ability to self-inject. Annals of Behavioral Medicine. 2001; 23(2): 125-32.
- Dashti Z, Sharifirad G, Hejazi SA, Mohebi S. The Effect of Training on Self-Care and Controlling Disease-Related Complications in Woman with Multiple Sclerosis: A Randomized Clinical Trial. J Qom Unv Med Sci. 2019; 13(1): 1-10. (Persian).
- Smrtka J, Caon C, Saunders C, Becker BL, Baxter N. Enhancing adherence through education. J Neuro Sci Nur. 2010; 42(5): S19-S29.
- Dashtian M, Eftekhar Ardebili H, Karimzadeh Shirazi K, Shahmoradi M, Azam K. Predicting factors affecting medication adherence and physical activity in patients with type-2 diabetes mellitus based on the theory of planned behavior. J Sch Pub Health Res. 2017; 15(2): 133-46. (Persian).
- Haker M, Heesen C, Wenzel L, Köpke S, Rahn AC, Kasper J. Decision-making about corticosteroids in relapses of multiple sclerosis - development of a questionnaire based on the theory of planned behaviour. Mult Scler Relat Disord. 2021; 55: 103182. doi: 10.1016/j.msard.2021.103182. Epub 2021 Jul 31. PMID: 34358850.
- Armitage CJ. Can the theory of planned behavior predict the maintenance of physical activity? Health psychology. 2005; 24(3): 235.
- Dinesh K Upadhyay SP PRS, Pranaya Mishra. Knowledge, Attitude and Practice about Diabetes among Diabetes Patients in Western Nepal. Rawal Med J. 2008; 33: 8-11.
- Gerber B, Cowling T, Chen G, Yeung M, Duquette P, Haddad P. The impact of treatment adherence on clinical and economic outcomes in multiple sclerosis: real world evidence from Alberta, Canada. Multiple sclerosis and related disorders. 2017; 18: 218-24.
- Filipi M, Jack S. Interferons in the Treatment of Multiple Sclerosis: A Clinical Efficacy, Safety, and Tolerability Update. J Int of MS Care. 2020; 22(4): 165-72.
- Jones JL, Scheidt DJ, Kaushal RS, Carroll CA. Assessing the role of patient support services on adherence rates in patients using glatiramer acetate for relapsing-remitting multiple sclerosis. J Med Eco. 2013; 16(2): 213-20.
- Mohammadpour N, Tabas EE. Effect of self-management program on treatment adherence in patients with multiple sclerosis. J Med Sur Nur. 2017; 6(1). (Persian).
- Burke T, Dishon S, McEwan L, Smrtka J. The evolving role of the multiple sclerosis nurse: an international perspective. J Int MS Care. 2011; 13(3): 105-12.
- Zimmer A, Bläuer C, Coslovsky M, Kappos L, Derfuss T. Optimizing treatment initiation: effects of a patient education program about fingolimod treatment on knowledge, self-efficacy and patient satisfaction. Multiple sclerosis and related disorders. 2015; 4(5): 444-50.
- Khan F, Pallant JF. Use of International Classification of Functioning, Disability and Health (ICF) to describe patient-reported disability in multiple sclerosis and identification of relevant environmental factors. J Reh Med. 2007; 39(1): 63-70.
- Saunders C, Caon C, Smrtka J, Shoemaker J. Factors that influence adherence and strategies to maintain adherence to injected therapies for patients with multiple sclerosis. J Neu Nur. 2010; 42(5): S10-S8.
- Goldoust F, Garmaroudi G, Abolhasani M, Shakibazadeh E, Yaseri M. Determinants of physical activity in women with multiple sclerosis based on theory of planned behavior. J Family Med Prim Care. 2022; 11(3): 1077-1082. doi: 10.4103/jfmpc.jfmpc_461_21. Epub 2022 Mar 10. PMID: 35495780; PMCID: PMC9051671.
- Kasser SL, Rizzo T. An exploratory study of fitness practitioner intentions toward exercise programming for individuals with multiple sclerosis. Disabil Health J. 2013; 6(3): 188-94. doi: 10.1016/j.dhjo.2012.12.002. Epub 2012 Dec 25. PMID: 23769477.
- Dhib-Jalbut S, Markowitz C, Patel P, Boateng F, Rametta M, Group SS. The combined effect of nursing support and adverse event mitigation on adherence to interferon beta-1b therapy in early multiple sclerosis: the START study. J Int MS Care. 2012; 14(4): 198-208.
- Ajzen I, Czasch C, Flood MG. From Intentions to Behavior: Implementation Intention, Commitment, and Conscientiousness 1. Journal of Applied Social Psychology. Wiley Online Library. 2009; 39(6): 1356-72. doi:10.1111/j.1559-1816.2009.00485.X.
- Ajzen I. The theory of planned behavior. Organizational behavior and human decision processes. Elsevier. 1991; 50(2): 179-211. doi: 10.1016/0749-5978(91)90020-T.
- Ajzen I. Constructing a TPB Questionnaire. Conceptual and Methodological Considerations. Retrieved from http://www.people.umass.edu/aizen/pdf/ tpb.measurement.pdf. (Last access August 2011). 2006.
- Kasper J, Köpke S, Fischer K, Schäffler N, Backhus I, Solari A, Heesen C. Applying the theory of planned behaviour to multiple sclerosis patients’ decisions on disease modifying therapy – questionnaire concept and validation. BMC Medical Informatics and Decision Making. 2012; 2(12): 60.