Case Series
Volume 3, Issue 2
Dermoscopy in the Diagnosis of Darier’s Disease: A Precise Approach
Kaoutar Mejjati1*; Zakia Douhi1; Souhaila El Yaagoubi2; Meryem Soughi1; Sara Elloudi1; Hanane Baybay1; Layla Tahiri EL Ousrouti2; Fatima Zahra Mernissi1
1Department of Dermatology, University Hospital Hassan II, Fez, Morocco.
2Pathology Department, University Hospital Hassan II, Fez, Morocco.
Corresponding Author :
Mejjati Kaoutar
Tel: +212-618332322;
Email: kaoutarme@hotmail.fr
Received : Jan 18, 2024 Accepted : Feb 16, 2024 Published : Feb 23, 2024 Archived : www.meddiscoveries.org
Citation: Mejjati K, Douhi Z, Yaagoubi SE, Soughi M, Elloudi S, et al. Dermoscopy in the Diagnosis of Darier’s Disease: A Precise Approach. Med Discoveries. 2024; 3(2): 1123.
Copyright: © 2024 Mejjati K. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Darier’s disease, a rare genetic condition with autosomal transmission that alters keratinization, clinically manifests as pruritic keratotic papules, mainly localized on seborrheic areas. Due to the similarity in presentation with other pathologies, dermoscopy plays a crucial role in diagnostic orientation. We report two observations of patients with Darier’s disease, highlighting distinctive dermoscopic structures, such as brownish polygonal areas surrounded by a whitish halo, thus contributing to a more accurate diagnosis.
Introduction
Darier’s disease, known as “Darier follicular keratosis” or “Darier-White disease,” is a relatively rare autosomal dominant genetic disorder. Clinically, it presents with keratotic papules, giving a rough appearance to the skin, with dermoscopic features being less explored. Through these two case observations, we will highlight the dermoscopic aspects in two patients with Darier’s disease.
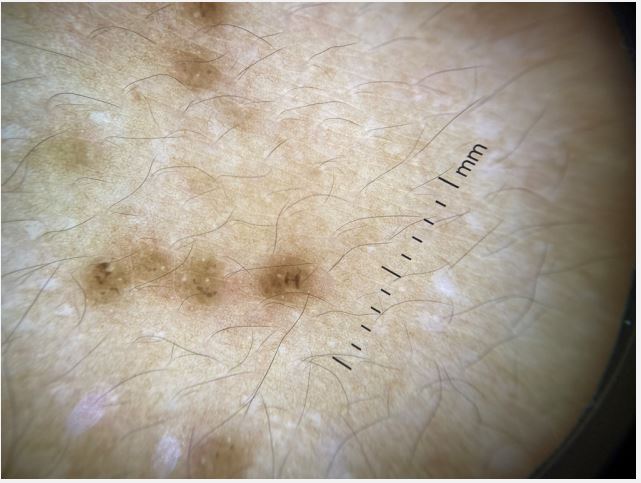
Observation 1: Mr. A, 22 years old, with no notable medical history, presented with a mildly pruritic skin rash evolving for 2 years on the trunk and back. Clinical examination revealed pigmented keratotic papules (Figure 1). Dermoscopy revealed brownish polygonal structures surrounded by a whitish halo (Figure 2). Biopsy confirmed acantholytic and keratotic epidermis, with intra-epidermal detachment forming cavities containing clear content, dyskeratotic cells, and round bodies, suggesting Darier’s disease.
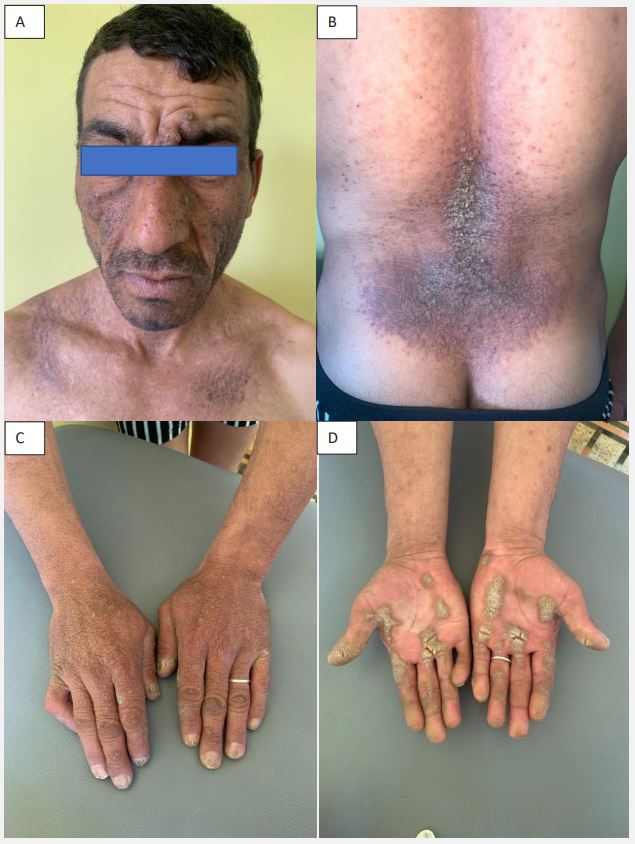
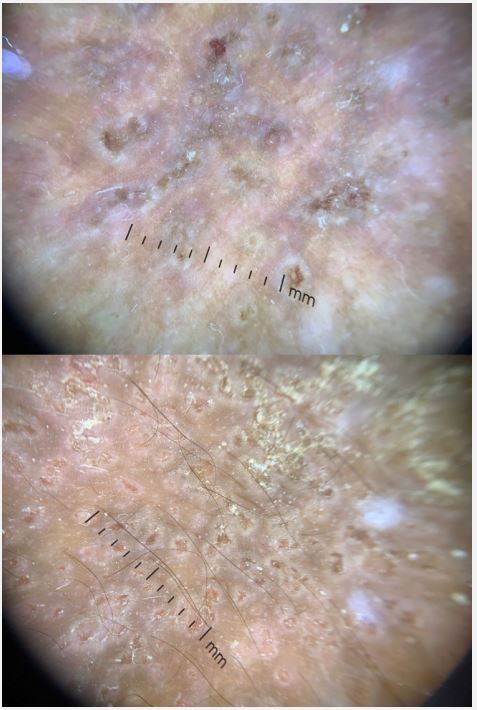
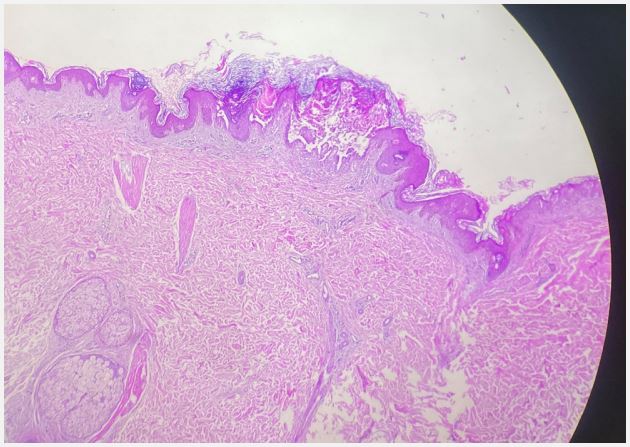
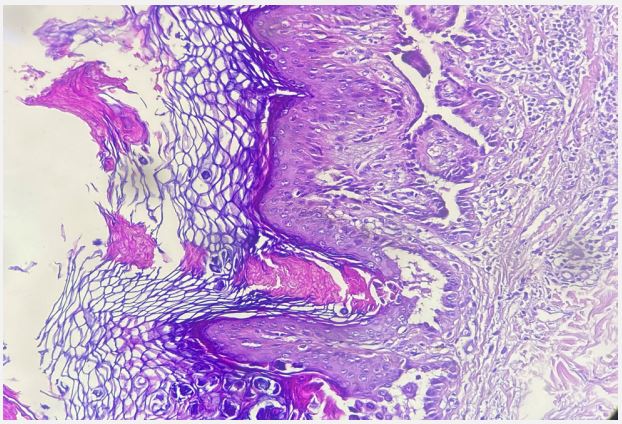
Observation 2: Mr. M, 39 years old, with no notable medical history, sought consultation for pruritic malodorous lesions evolving for 12 years. Dermatological examination revealed hyperpigmented verrucous plaques with keratotic surfaces in the axillary, inguinal, intergluteal, retroauricular, lumbosacral, facial, and neck regions. Fissured palmoplantar keratoderma was also present. Nail examination showed subungual hyperkeratosis and diffuse trachyonychia (Figure 3). Dermoscopy of the skin lesions revealed central keratin and brownish areas without structures surrounded by whitish radial streaks, and peripheral vascularization (Figure 4). Biopsy showed acanthotic epidermis with orthokeratotic hyperkeratosis, focal intra-epidermal acantholysis, suggesting Darier’s disease (Figures 5 and 6).
Discussion
Darier’s disease is a chronic acantholytic and dyskeratotic dermatosis, resulting from a keratinization disorder, first described by Jean Darier and James Clarke White in 1889 [1]. It is caused by a loss of interkeratinocyte adhesion due to a mutation in the ATP2A2 gene, encoding a protein involved in calcium transport inside cells. It typically manifests in childhood or adolescence, affecting both sexes equally [2].
Clinically, Darier’s disease presents with erythematous or brownish keratotic and pruritic papules, which coalesce into extensive plaques, often affecting seborrheic regions, including the trunk, scalp, face, and neck, giving the skin a rough, dirty, and malodorous appearance [3]. Palmoplantar keratoderma and nail anomalies such as trachyonychia, subungual hyperkeratosis, subungual hemorrhages, and V-shaped distal notching may also be observed.
Dermoscopy of Darier’s disease was first described in 2004 by Vázquez-López [4]. Currently, there is limited literature on dermoscopy for this condition. Reported dermoscopic features include yellowish-brown polygonal or star-shaped structures in the center, surrounded by a whitish halo, on a homogeneous pink background, with peripheral point or linear vascularization [5]. Histologically, the central yellow-brown area surrounded by a whitish halo corresponds to compact hyperkeratosis and acanthosis. The erythematous background correlates with chronic inflammation [5,6].
Darier’s disease is characterized histologically by acantholysis, loss of cellular adhesion, and dyskeratosis with the formation of round bodies in the granular layer and grains primarily in the corneal layer. There is no curative treatment for the disease. Management aims to relieve symptoms, emphasizing hygiene measures such as photoprotection, wearing cotton clothing, using emollients and keratolytics based on urea or lactic acid. Oral retinoids may also be used in extensive forms [7].
Conclusion
Darier’s disease tends to be confused with other dermatological conditions and is often misdiagnosed, highlighting the importance of dermoscopy in guiding the diagnosis.
Consent: Patient examinations were conducted in accordance with the principles of the Helsinki Declaration.
Conflicts of interest: The authors declare no conflicts of interest.
References
- Engin B, Kutlubay Z, Erkan E, Tüzün Y. Darier disease: A fold (intertriginous) dermatosis. Clin Dermatol. 2015; 33: 448-451.
- Dhitavat J, Fairclough RJ, Hovnanian A, Burge SM. Calcium pumps and keratinocytes: Lessons from Darier’s disease and Hailey‐Hailey disease. Br J Dermatol. 2004; 150: 821‐8.
- Buteică E, Burada F, Stoicescu I, Stănoiu B, Georgescu CV. Darier disease and Hailey-Hailey disease. Rom J Morphol Embryol. 2007; 48: 423-6.
- Vázquez-López F, Lopez-Escobar M, Maldonado-Seral C, PerezOliva N, Marghoob AA. The handheld dermoscope improves the recognition of giant pseudocomedones in Darier’s disease. J Am Acad Dermatol 2004; 50(3): 454-5.
- Errichetti E, Stinco G, Lacarrubba F, Micali G. Dermoscopy of Darier’s disease. J Eur Acad Dermatol Venereol. 2016; 30(8): 1392-4.
- Lacarrubba F, Verzì AE, Errichetti E, Stinco G, Micali G. Darier disease: Dermoscopy, confocal microscopy, and histologic correlations. J Am Acad Dermatol 2015; 73(3): 97-9.
- Valois P-Y, Girault, J-J, Morand. Maladie de Darier. EMC – Dermatologie. 2016; 11: 1-9.