Research Article
Volume 3, Issue 2
Social Determinants of Health Services Utilization Among Patient with Chronic Diseases Based on the China Health and Retirement Longitudinal Survey
Cheng Cong; Xiao Lei; Yang Jian; Hu Qian; Yang Yuan; Zhang Fan*
School of Public Health and Management, Chongqing Medical University, Chongqing, 400016, China.
Corresponding Author :
Zhang Fan
Tel: +86-13983782377, Fax: 0086-023-68485068;
Email: zhangfan@cqmu.edu.cn
Received : Jan 12, 2024 Accepted : Feb 13, 2024 Published : Feb 20, 2024 Archived : www.meddiscoveries.org
Citation: Cong C, Lei X, Jian Y, Qian H, Fan Z, et al. Social Determinants of Health Services Utilization Among Patient with Chronic Diseases Based on the China Health and Retirement Longitudinal Survey. Med Discoveries. 2024; 3(2): 1120.
Copyright: © 2024 Fan Z. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Objective: In a word, the published studies are about health services among different population groups. Moreover, most of these studies focused on the relationship between medical insurance and health services, without utilizing the latest data and large sample sizes. This study aims to evaluate health services and their associated factors among middle-aged and elderly people with chronic diseases in China.
Methods: This cross-sectional study utilized data from the China Health and Retirement Longitudinal Study (CHARLS) conducted in 2020 by the National School of Development of Peking University. Weighted percentages were used to describe the characteristics of the middle-aged and elderly chronic patient population, ensuring representation at national and domain levels. Pearson’s chi-square test was employed to examine the association between social determinants and health services. Andersen’s health services model and binary logistic regression were used to evaluate the determinants of health services utilization among middle-aged and elderly individuals with chronic diseases.
Results: The study sample consisted of 19,103 participants who completed the questionnaire. Residence and sex were found to be influencing factors for outpatient and inpatient services, respectively. Regarding health services, predisposing factors such as age, sex, individual income, self-reported health, presence of chronic disease, and alcohol consumption significantly affected health services utilization in this population. Enabling factors indicated that individuals with middle and high incomes reported lower utilization of health services compared to those with low incomes. Among demand factors, individuals with fewer chronic diseases and good self-rated health were found to significantly reduce their use of health services, while abstaining from alcohol increased the utilization of medical services.
Conclusion: Policymakers in China may need to further adjust healthcare policies. Specifically, health promotion efforts should be targeted towards elderly women with low incomes to enhance their awareness and utilization of health services, thereby improving overall utilization rates.
Keywords: Social determinants; Health services; Chronic disease; Elderly.
Introduction
Due to the rapidly ageing population and increasing longevity, a growing number of people are living for long periods of time with chronic disease. The World Health Organization (WHO) reported that chronic diseases kill 40 million people per year, which is equivalent to 70% of all deaths globally [1]. Chronic diseases not only have a long course, but also have a poor prognosis. In recent years, the incidence of chronic diseases has increased year by year, making it the main cause of death in our country and the primary public health problem affecting people’s health [2].
Chronic diseases have become a major cause of death for the world’s population today. According to the world health statistics 2023 by WHO, NCDs (Noninfectious Chronic Disease) continued to cause the highest disease burden worldwide. The impact of NCDs grew from causing 61% of global deaths (equivalent to 31 million) in 2000 to causing 74% (or 41 million) in 2019. Globally, the greatest decline in deaths from major NCDs between 2000 and 2019 were from chronic respiratory disease [3]. Chronic diseases already account for more than 80% of all deaths among our residents nationwide.
Over the years, the utilization of services for patients with chronic diseases, outpatients and inpatients has been widely concerned. Compared with healthy people, the proportion of outpatients and inpatients with chronic diseases is higher. However, the demand and utilization of health services for patients with chronic diseases in China do not match, which is reflected in two aspects: insufficient utilization and low quality of services. Middle-aged and elderly people are a period of high incidence of chronic diseases, and the deepening of aging will inevitably lead to an increase in the demand for health services. The demand for chronic disease treatment and health services among middle-aged and elderly people is much higher than that of other people [4].
Anderson model was first designed to study the influence of medical and health services utilization behavior, which is widely used in the utilization of medical services for the elderly abroad, and has now been applied in many parts of the health system involving different diseases [5].
The utilization of health services is a complex behavior, and obtaining health services depends not only on the health status of individuals, but also on the demand generated by social determinants. Mechanic, an American scholar, believes that the utilization of health services is the behavior that patients explore and predict their own health status through various methods and channels, and consume various medical resources to treat diseases [6].
Many domestic scholars believe that the utilization of health services is to improve their own health medical service demand and supply, and often use outpatient service and inpatient service to represent the utilization of health services [7]. Policymakers and health services providers need to investigate and understand the determinants of health services utilization for the elderly, optimize the allocation of health services resources, and thus improve the level of health services utilization [8].
The overall goal of this study was to analyses the current situation of health services and social determinants and its associated factors among middle-aged and elderly people with chronic conditions to provide an empirical basis for research on the direction of health services of chronic disease patients in China. It aims to improve the utilization of health services and provides theoretical support for policy formulation by relevant government departments. Two specific objectives were defined: (1) To describe the current situation of health services and social determinants (2) To use Anderson’s behavior model, to identify factors associated with health services among middle-aged and elderly individuals with chronic diseases [9].
Data and methods
Data source
This study utilized data from the China Health and Retirement Longitudinal Survey (CHARLS;https: //charls.charlsdata. com/pages/Data/2020-charls-wave5/zh-CN.html) in 2020 [10]. The CHARLS fifth national follow-up data for 2020 was officially released on November 16th, 2023. The China Health and Retirement Longitudinal Survey aims to collect high-quality microdata representing families and individuals aged 45 and above in China [11]. The national baseline survey was conducted in 2011, with survey visits taking place in 150 counties and 450 communities (villages) in 28 provinces (autonomous regions and municipalities directly under the Central Government) in 2011, 2013, 2015 and 2018 respectively. By the time the nationwide follow-up visit was completed in 2018, the sample had covered 19,000 respondents from a total of 12,400 households [12].
To ensure unbiased and representative samples, a multistage stratified probability proportional sampling was employed, with direct sampling at the county level (counties or urban areas). These counties cover 28 of 30 provinces in mainland China, excluding Tibet [13]. The sampling process was conducted using STATA and SPSS no sample changes were allowed.
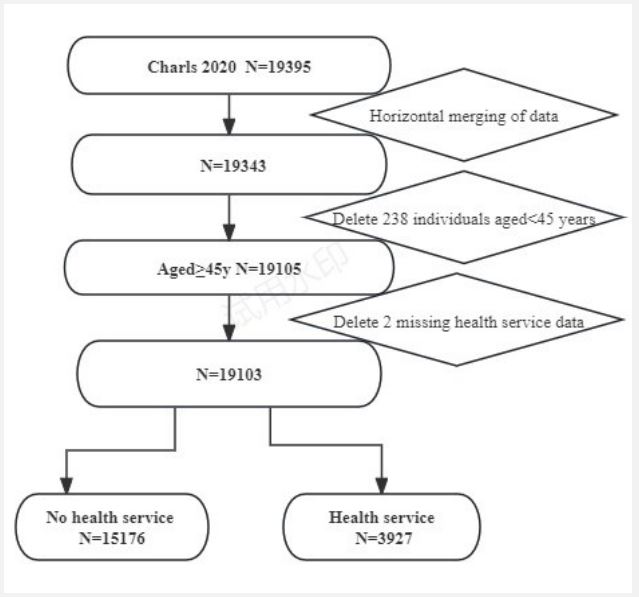
CHARLS baseline data includes some information about respondents and dropouts. The main questionnaire consists of basic demographic statistics, family, health status and function, work and retirement, income and expenditure epidemic situation and other information. In the fifth wave of survey in 2020, there were 19,395 respondents with baseline data. For this paper, 238 individuals under the age of 45 and two individuals without health services information were excluded, resulting in a total of 19,103 observations included in the analysis.
Statistical analysis: The participants provided written informed consent before participating in the study.
The utilization of health services refers to the number of people who need health services and actually use them. The dependent variable is health services, which is embodied by outpatient service and inpatient service.
The dependent variable ʻoutpatient service’ was dichotomised into 0=ʻnever visited a medical institution for outpatient visits or received inpatient services in the past month’ and 1=ʻhave visited a medical institution for outpatient visits or received inpatient services in the past month’. The dependent variable ʻ inpatient service’ was dichotomised into 0=ʻnever hospitalized in the past year’ and 1=ʻhave hospitalized in the past year?’. Regarding whether they have received health services, considering that the respondents might have received outpatient services or inpatient services before taking part in the survey, as long as the answer of outpatient service or inpatient service is yes, it will be recorded as 1, and if not, it will be recorded as 0 [14].
The patients with chronic diseases over 45 years old who answered the health services question were selected in the China Health and Retirement Longitudinal Survey. The data screening process was shown in Figure 1.
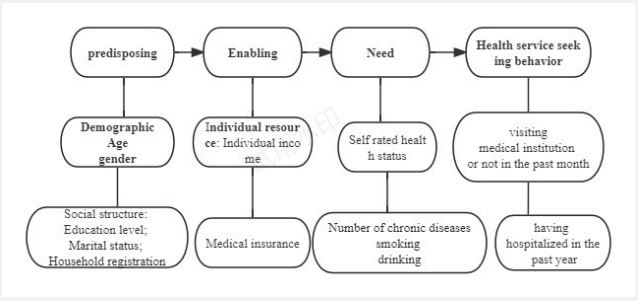
Based on the Anderson model, two core dimensions, personal characteristics and medical behavior, were constructed to build a theoretical framework. Personal characteristics included tendency factors, enabling factors and demand factors that affected the health services of middle-aged and elderly chronic patients. Medical behavior included outpatient medical treatment and hospitalization service. The Anderson model was illustrated in Figure 2.
Variable selection: The dependent variables were two types of health services: outpatient services and inpatient services. Participants were asked the following two questions: “Have you been ill in the last month?” and “What was the main reason for not seeking outpatient treatment?”, and the responses were used to estimate “non-use of outpatient services” (i.e. if the participant answered that they had been ill but did not seek medical treatment). Participants were also asked, “In the past year, did a doctor suggest that you needed inpatient care but you did not get hospitalized?” and the response was used to estimate “non-use of inpatient services” (i.e. if the participants answered that they did not go to the hospital when a doctor had suggested the need for inpatient services) [15].
Independent variables were selected based on Andersen’s healthcare utilization model (a behavior model). This model suggests that the use of health services in an individual is determined by three key factors: predisposing, enabling, and need factors.
In our analysis, we included age, sex, marital status, area of residence (Hukou), and education level as social structure factors. Predisposing factors include demographic characteristics and social structure. Age was divided into three groups with a 15-year interval, and the last group consisted of individuals over 75 years old. Marital status was divided into two groups: married and cohabiting, and other marital statuses. Area of residence uses household registration instead of area of residence, and household registration is divided into two categories: rural household registration and non-rural household registration. Education level is divided into four groups: less than primary school, less than lower secondary, upper secondary and vocational training, and tertiary education.
Enabling factors are those that make health services resources available to an individual; they can be measured by individual income and health insurance. Individual income is calculated as the sum of personal salary and transfer payment income. Then according to the income trinket, the subjects were divided into three groups: lowincome group, middle income group and high income group. Medical insurance is divided into four types: UEMI, NCMI, URMI and Others insurance. Need factors represent the demand for health care services, including self-reported health status and the number of chronic diseases, as well as lifestyle such as smoking and drinking. The number of chronic diseases can be divided into three categories: those who are not sick, those who suffer from one chronic disease and those who suffer from many chronic diseases [16]. Variables included in the multivariate model are presented in Table 1.
Results
Bivariate correlation analyses: Table 2 shows the results of comparison of health services and sociodemographic characteristics by inpatient and outpatient care utilization in 2020. The following characteristics were associated with greater likelihood of outpatient care: age, area of residence, the types of medical insurance, income level, self-report health status, the number of chronic disease, drinking behavior. Similarly, the following characteristics were associated with greater likelihood of inpatient care: sex, age, the types of medical insurance, income level, self-report health status, the number of chronic disease, drinking behavior.
Sample characteristics and associations between social determinants and health services: Descriptive statistics of the samples evaluated are shown in Table 3. The total sample consisted of 19103 respondents ≥45 years old. The missing data in the independent variables are compensated by linear interpolation. Of the 19103 participants (9034 man and 10069 woman), 14484 (75.82%) were married and partnered. The participants ranged in age from 45 to 108 years (mean 61.81±9.84), with 44.38% between the ages 45 to 59. More than 90% (18183) were primary school and below, nearly three-fourths (74.53%) stayed in a rural residence, nearly three-fourths (14238) had new cooperative medical insurance. There are 6536 (34.21%) people with high income. At most, 8741 (45.76%) rated their health as fair. No chronic diseases accounted for 11,846 (62.01%). Among them, 12,244 (64.09%) never drank,18688 (97.83%) smoked.
As shown in Table 3, the results of the Chi-square test indicated that the sociodemographic characteristics of health services prevalence was different according to various independent variables. For the predisposing factors, a higher proportion of woman, older individuals had utilized of health services (both P<0.05). Concerning the enabling factors, those with middle income (P<0.05) seemed to make more use of health services. As for the need factors, individuals with poor health status and more chronic diseases tended to use health services more frequently. Moreover, individuals without habits of alcohol drinking reported a higher rate of use of health services (both P<0.05).
Fit coefficients of models: According to the traditional modeling method of Anderson’s model, the factors of P<0.05 in Table 3 were included in the Logistic regression analysis. Model 1 included propensity factors alone, model 2 included propensity factors and enabling factors, and model 3 included demand factors on the basis of model 2. As shown in Table 4, from Model 1 to Model 3, Cox& Snell R2 and Nagelkerke R2 and their increase gradually increased, and the value of -2LL was decreased, which indicated that Model 3 had the best fitting effect.
Binary logistic regression analysis of health services: OR (95% CI): Compared with people aged from 45 to 60, those aged from 60 to 75 and those older than 75 were 0.76 and 0.98 times respectively (OR=0.764, 95% CI: 0.688 to 0.849), (OR=0.985, 95% CI: 0.889 to 1.092). Women who use health services were 0.98 times that of men (OR=0.981, 95% CI: 0.941 to 1.053), and that of middle income (1,000 to 10,000) were 1.10 times that of low income (<1,000) (OR=1.107, 95% CI: 1.023 to 1.198), the odds ratio for high income (≥10,000) individuals was 1.04 times that of lowincome individuals. Compared to those who self-reported their health as very good, those who self-reported their health as good and very poor were 0.160 and 0.641 times more likely, respectively (OR=0.160, 95% CI: 0.134 to 0.190), (OR=0.641, 95% CI: 0.561 to 0.733). Compared to those without chronic diseases, those with one chronic disease and those with many chronic diseases had odds ratios of 0.35 and 0.66, respectively (OR=0.354, 95% CI: 0.323 to 0.388), (OR=0.657, 95% CI: 0.594 to 0.726), Compared to those who drink alcohol, people who never drink alcohol were 1.21 times more likely to use health services (OR=1.210, 95% CI: 1.122 to 1.305).
Discussion
With the rapid aging of the population in China, the number of chronic diseases continues to rise, and the elderly are facing health services challenges. To our knowledge, this is the first article to analyze the data of health services among patients with chronic diseases in the national and representative China Health and Retirement Longitudinal Survey in 2020. Our findings contribute to a comprehensive understanding of the social determinants of health services, which might provide valuable insights for designing policies and improving the population’s health perceptions and responsible use of health services.
The results showed that when comparing the differences between social determinants and health services, we found that residence was the influencing factor of outpatient service, and sex is the influencing factor of inpatient service. Considering the economy and convenience of medical treatment [17], rural areas might prefer outpatient service, and women who were unwell might prefer to be hospitalized. Of all the respondents, 52.71% were women, 44.38% were aged 45 to 59, and 75.82% were married or in a companionship, 95.18% had an education level lower than junior high school, 74.53% were in rural areas, 74.45% used the new rural cooperative medical insurance, 34.21% had a high income, and 44.21% had a low income. 64.09% of the respondents did not drink alcohol. 97.83% of the respondents were smokers. The proportion of people aged 45- 59 using health services was 27.34%, that of people aged 60 to 74 was 35.90%, and that of people over 75 was 39.73%. It showed that the proportion of using health services was increasing with age, and self-reported health and the number of chronic diseases were also increasing. Other factors were similar, and the proportion of drinkers using health services was lower than that of non-drinkers. People who drink alcohol might feel better about themselves or be in better health [18,19].
Among predisposing factors, our results indicate that the possibility of using health services increases with increasing age. This finding is consistent with previous literature reports [20,21]. Patients with chronic diseases aged 45 to 59 had the highest probability of using health services compared to other age groups. This can be attributed to the fact that this group experiences milder symptoms of chronic diseases and tends to seek medical treatment more frequently [22]. Moreover, we found that sex is associated with the use of health services. The possibility of women using health services was 0.99 times that of men, indicating that the utilization rate of health services is similar between men and women, with a slightly higher preference for men, possibly due to a higher incidence of illness among men [23]
In terms of income levels, the possibility of individuals with middle and high incomes utilizing health resources was 1.11 times and 1.04 times that of those with low incomes, respectively. This may be due to the fact that individuals with higher incomes have more financial resources to allocate towards healthcare and are more likely to face health issues as a result [24]. Our findings align with previous studies that have shown a positive correlation between higher income levels and the utilization of health services. “No money” was reported as the main reason for not using health services [25]. Additionally, the utilization rate of health services increases as economic levels improve. Therefore, economic factors play a significant role in determining the utilization of health services [26,27].
Another important factor influencing the use of health resources is health status, which is more accurately assessed through self-reported of health. Compared to individuals who reported their health as “very good,” those who reported their health as “very poor” had a utilization rate that was 0.641 times lower, while those with poor health had a utilization rate that was 0.208 times lower. These findings are consistent with previous research conducted by other scholars [28].
Compared with patients without chronic diseases, those with one chronic disease and those with multiple chronic diseases were 0.35 and 0.657 times more likely to use health services. The results were consistent with other studies [29,30]. The possible reasons were: one was that people with poor health might be poor health. They must use health services to improve the symptoms of the disease. On the other hand, people with more diseases might need more health resources and use health services for medical treatment for emerging health problems [31].
Finally, in terms of the relationship between drink and health services, there were 12244 (64.09%) older adults who reported that respondents almost did not drink among in 2020. It was a personal healthy behavior to drink [32]. The results demonstrated a strong association between drank and health services. Compared with those who drank, those who didn’t drink were 1.210 times more likely to use health services. The possible reason was that the alcohol treatment strategy of drinkers had a positive impact on reducing the utilization rate of health services. The results were consistent with other people’s research [33].
Limitations of the study: There were limitations in interpreting the results of the study. Firstly, the data in CHARLS came from a large cohort study. Second, the data for some of the factors were derived from respondents’ self-reported of health, which might lead to recall bias or reporting bias. Finally, the cross-sectional data cannot be used to prove any causal relationships between social determinants and health services.
Conclusion
In summary, the utilization rate of health services in people over 75 years old was 39.73% and was increasing over the years. Health services was strongly associated with several factors such as age, sex, individual income level, self-reported of health, the number of chronic diseases, drink. In order to improve the utilization rate of health services, elderly women with low income should be given health publicity to improve their awareness of using health services. For people who have self-reported good health, suffer from a chronic disease, and drink, they should use health services according to the actual situation and give full play to the functions of health services. Finally, further longitudinal studies are needed to understand the causal relationships between health services and social determinants.
Strengths and limitations of this study: This study represents the first analysis of health services data among patients with chronic diseases using the national and representative China Health and Retirement Longitudinal Survey in 2020.
The China Health and Retirement Longitudinal Study is the first national survey focusing on middle-aged and elderly individuals. Andersen’s model was utilized to examine social determinants of health services utilization, and comparison with past results guided policy choices. Cross-sectional studies cannot establish causal relationships. Some health services indicators have a one-year time span, which may introduce recall bias.
Declarations
Acknowledgements: The authors thank the National School of Development, Peking University and other members for their support and cooperation.
Funding: No specific funding was received for this work.
Conflicts of interest/competing interests: The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethics approval: This study was approved by the Ethics Committee of Chongqing Medical University (No. (2021)013) and in accordance with the Declaration of Helsinki.
Consent to participate: Participants were fully informed regarding the survey prior to participation. Completing and submitting the questionnaire was considered a proxy consent to participate. In this study, all participants were voluntary and the questionnaire was anonymous, we also used non-identifying codes, ensuring the confidentiality of the information.
Authors’ contribution statements: All authors contributed to the study conception and design. The manuscript writing for the original draft and data analysis were completed by Cheng Cong. Yang Jian gave the paper revision and format adjustment work. The rest of the authors gave the paper revision. Zhang Fan and Yang Yuan gave the entire process technical and paper writing guidance support. All authors read and approved the final manuscript. All authors read and approved the final manuscript.
References
- Li X, Chen M, Wang Z, Si L. Forgone care among middle aged and elderly with chronic diseases in China: evidence from the China Health and Retirement Longitudinal Study Baseline Survey. BMJ Open. 2018; 8(3): e019901.
- Chen L, Gong Y, Yuan L. Health behavior and its determinants in elderly patients with chronic diseases: evidence from Jiangsu Province, China. BMC Geriatr. 2022; 22(1): 297.
- World health statistics 2023: monitoring health for the SDGs, Sustainable Development Goals. Geneva: World Health Organization. Licence: CC BY-NC-SA 3.0 IGO. 2023.
- Hopman P, Schellevis FG, Rijken M. Health-related needs of people with multiple chronic diseases: differences and underlying factors. Qual Life Res. 2016; 25(3): 651-660.
- Xin Y, Ren X. Determinants of province-based health services utilization according to Andersen’ s Behavioral Model: a population-based spatial panel modeling study. BMC Public Health. 2023; 23(1): 985.
- Alkhawaldeh A, ALBashtawy M, Rayan A, et al. Application and Use of Andersen’s Behavioral Model as Theoretical Framework: A Systematic Literature Review from 2012-2021. Iran J Public Health. 2023; 52(7): 1346-1354.
- Lu P, Yang C, Yao J, Shelley M. Outpatient and Inpatient Service Use by Chinese Adults Living in Rural Low-Income Households. Soc Work Public Health. 2020; 35(4): 223-233.
- Pérez-Escamilla R, Engmann C. Integrating nutrition services into health care systems platforms: Where are we and where do we go from here. Matern Child Nutr. 2019;15-1(1): 12743.
- Li X, Chen M, Wang Z, Si L. Forgone care among middle aged and elderly with chronic diseases in China: evidence from the China Health and Retirement Longitudinal Study Baseline Survey. BMJ Open. 2018; 8(3): 019901.
- Wu X, Li X, Xu M, Zhang Z, He L, Li Y. Sarcopenia prevalence and associated factors among older Chinese population: Findings from the China Health and Retirement Longitudinal Study. PLoS One. 2021; 16(3): 0247617.
- Zhao X, Zhou Y, Wei K, et al. Associations of sensory impairment and cognitive function in middle-aged and older Chinese population: The China Health and Retirement Longitudinal Study. J Glob Health. 2021; 11: 08008.
- Wang HY, Meng Q, Yang C, et al. Association between pulse pressure, systolic blood pressure and the risk of rapid decline of kidney function among general population without hypertension: results from the China health and retirement longitudinal study (CHARLS). J Transl Med. 2021; 19(1): 512.
- Yao SS, Cao GY, Han L, et al. Prevalence and Patterns of Multimorbidity in a Nationally Representative Sample of Older Chinese: Results From the China Health and Retirement Longitudinal Study. J Gerontol A Biol Sci Med Sci. 2020; 75(10): 1974-1980.
- Asamrew N, Endris AA, Tadesse M. Level of Patient Satisfaction with Inpatient Services and Its Determinants: A Study of a Specialized Hospital in Ethiopia. J Environ Public Health. 2020; 2020: 2473469.
- Shaqura II, Jaafaripooyan E, Ahmadi B, Akbari Sari A. Responsiveness of hospitals to inpatient and outpatient services in the low- and middle-income countries: A systematic review. Int J Health Plann Manage. 2022; 37(1): 78-93.
- Airhihenbuwa CO, Tseng TS, Sutton VD, Price L. Global Perspectives on Improving Chronic Disease Prevention and Management in Diverse Settings. Prev Chronic Dis. 2021; 18: E33. Published 2021 Apr 8.
- Zhu W, He J, Guo H. Doctor-patient bilateral matching considering diagnosis and treatment perception in the absence of public health resources. Front Public Health. 2023; 10: 1094523.
- Zhu W, He J, Guo H. Doctor-patient bilateral matching considering diagnosis and treatment perception in the absence of public health resources. Front Public Health. 2023; 10: 1094523. Published 2023 Jan 19.
- Zhao P, Wang LY, Zhao L. Can Sound Health Insurance Increase the Internal Circulation in the Economy of China?. Front Public Health. 2021; 9: 710633. Published 2021 Jul 15.
- Asmar S, Weinberg M, Bjorklund J, et al. The Impact of Age on the Epidemiology and Cost of Atrial Fibrillation Hospitalizations. Am J Cardiol. 2023; 205: 126-133.
- Stucki M, Schärer X, Trottmann M, Scholz-Odermatt S, Wieser S. What drives health care spending in Switzerland? Findings from a decomposition by disease, health service, sex, and age. BMC Health Serv Res. 2023; 23(1): 1149. Published 2023 Oct 25.
- Pel-Littel RE, Snaterse M, Teppich NM, et al. Barriers and facilitators for shared decision making in older patients with multiple chronic conditions: a systematic review. BMC Geriatr. 2021; 21(1): 112.
- Berzins SA, Bulloch AG, Burton JM, Dobson KS, Fick GH, Patten SB. Determinants and incidence of depression in multiple sclerosis: A prospective cohort study. J Psychosom Res. 2017; 99: 169-176.
- GBD 2019 Stroke Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. 2021; 20(10): 795-820.
- Smith DK, Murphy BA. Lower levels of education and household income mediate lower dental care utilization among survivors of early life cancers. Prev Med Rep. 2019; 14: 100868. Published 2019 Apr 12.
- Powell-Wiley TM, Baumer Y, Baah FO, et al. Social Determinants of Cardiovascular Disease. Circ Res. 2022; 130(5): 782-799.
- Huttunen-Lenz M, Raben A, Adam T, et al. Socio-economic factors, mood, primary care utilization, and quality of life as predictors of intervention cessation and chronic stress in a type 2 diabetes prevention intervention (PREVIEW Study). BMC Public Health. 2023; 23(1): 1666. Published 2023 Aug 30.28.
- Nascimento M, Cunha Soares F, Dahllöf G, Burgos Souto Maior G, Kvist T, Colares V. Determinants of self-perceived oral health in adolescents: A cross-sectional study. Int J Paediatr Dent. 2021; 31(2): 254-261.
- Shi W, Zhang T, Li Y, Huang Y, Luo L. Association between household air pollution from solid fuel use and risk of chronic diseases and their multimorbidity among Chinese adults. Environ Int. 2022; 170: 107635.
- Sinnige J, Braspenning J, Schellevis F, Stirbu-Wagner I, Westert G, Korevaar J. The prevalence of disease clusters in older adults with multiple chronic diseases--a systematic literature review. PLoS One. 2013; 8(11): 79641. Published 2013 Nov 11.
- Johnson EM, Possemato K. Problem recognition and treatment beliefs relate to mental health utilization among veteran primary care patients. Psychol Serv. 2021; 18(1): 11-22.
- Michel L, Conq E, Combs E, et al. Alcohol use by people in their seventies is not an exception: a preliminary prospective study. Br J Community Nurs. 2019; 24(3): 128-133.
- Romero-Rodríguez E, Amezcua-Prieto C, Morales Suárez-Varela M, et al. Patterns of Alcohol Consumption and Use of Health Services in Spanish University Students: UniHcos Project. Int J Environ Res Public Health. 2022; 19(10): 6158. Published 2022 May 18.