Case Report
Volume 3, Issue 2
Exploring Dens Invaginatus Types I and II: Diagnosis, Challenges, and Solutions - A Case Report
Hajer Zaghdoudi1,2*; Amira Kikly1,2; Nabiha Douki1,2
1Department of Dentistry, Sahloul University Hospital (Sousse, Tunisia), Faculty of Dental Medicine of Monastir, Tunisia.
2Oral Health and Orofacial Rehabilitation Research Laboratory (LR12ES11), Faculty of Dental Medicine of Monastir, University of Monastir, Tunisia.
Corresponding Author :
Hajer Zaghdoudi
Email: hajer_za@yahoo.com
Received : Dec 08, 2023 Accepted : Feb 02, 2024 Published : Feb 09, 2024 Archived : www.meddiscoveries.org
Citation: Zaghdoudi H, Kikly A, Douki N. Exploring Dens Invaginatus Types I and II: Diagnosis, Challenges, and Solutions - A Case Report. Med Discoveries. 2024; 3(2): 1115.
Copyright: © 2024 Zaghdoudi H. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Dens invaginatus is a common malformation of maxillary lateral incisors with varying anatomical features that impose challenges to diagnosis and treatment. It is considered a real clinical entity which, even if the tooth is clinically healthy, it can cause pulpal damages that can progress silently and lead to necrosis and its complications. The aim of this article is to expose a clinical case of patient with two types of dental invaginations; I and II incidentally discovered during a routine radiological examination, affecting the two permanent maxillary lateral incisors which are clinically healthy, and which required endodontic treatment following pulpal damages. The focus will be on the description of the clinical and radiological characteristics of this abnormality, the difficulties and the strategies employed to manage this clinical condition.
Keywords: Dens in dente; Dens invaginatus; Classification; Diagnosis; Treatment; Case report.
Introduction
The invaginated tooth (dens invaginatus, dens in dente), a term introduced in 1953 by “Von Hallet,” is a dental developmental anomaly or dysmorphogenesis first described by a dentist named “Socrates” in 1856 [1,2]. It results from a partial invagination of variable depth of the enamel organ during tooth development [1]. This malformation leads to external modifications of dental anatomy, creating areas that are difficult to access for hygiene practices and become prime sites for bacterial stagnation, the development of carious lesions, and pulp involvement that can silently progress to necrosis and its complications, necessitating endodontic treatment [1]. The internal structural variations inherent in this dental disorder further complicate conventional endodontic treatment, a situation that has led to the development of new therapeutic procedures for treating these teeth [3]. In this context, we present a clinical case of two types of dens invaginatus, I and II, affecting both maxillary permanent lateral incisors, which were clinically healthy but required endodontic treatment due to pulpal diseases caused by this rare anomaly. Emphasis will be placed on the diagnostic and endodontic treatment challenges associated with these dens in dente.
Clinical case
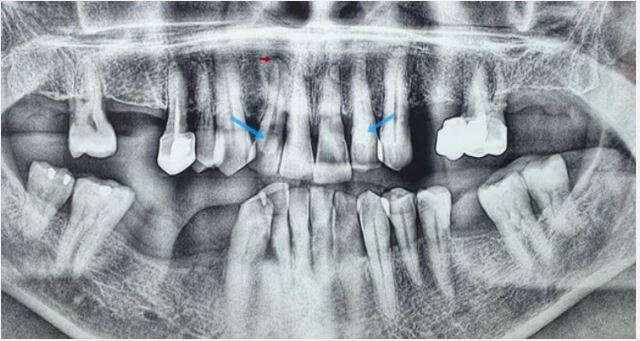
A 67-year-old patient with acute renal insufficiency, gastric ulcer, and Sjogren’s syndrome was referred to the Department of Dentistry at CHU Sahloul, Sousse, Tunisia, for a biopsy of the accessory salivary glands. The panoramic radiograph (Figure 1) revealed radiopaque enamel-like structures located at the cervical third of the crowns of right maxillary lateral incisor [12] and left maxillary lateral incisor [22], suggesting a dental malformation. Additionally, a radiolucent periapical image related to the root of tooth 12 was observed. This prompted us to further investigate our clinical examination.
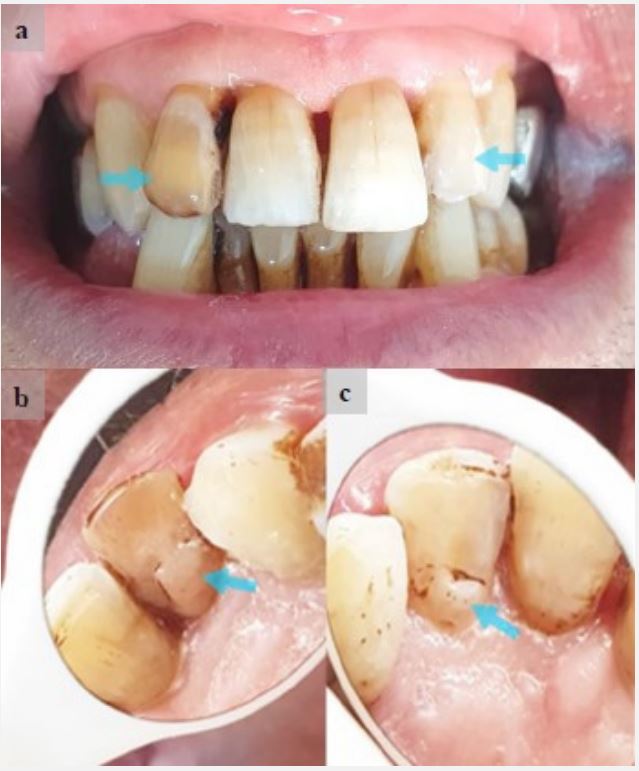
On a frontal view, the examination revealed an oval shape of the crowns of both maxillary lateral incisors, discoloration of tooth 12 concealed by moderate fluorosis, and the absence of carious lesions (Figure 2a). On a palatal view, an enlarged cingulum in the form of a tubercle and an accentuated cingulum pit suggested dental invagination (Figure 2b and 2c).
a) Frontal View: Teeth exhibit moderate fluorosis, both lateral incisors have an oval shape with no carious lesions, and there is discoloration of tooth (12). b) Palatal View of Tooth (12): Pronounced cingulum with an accentuated cingulum pit in the form of a tubercle. c) Palatal View of Tooth (22): Pronounced cingulum with an accentuated cingulum pit in the form of a tubercle.
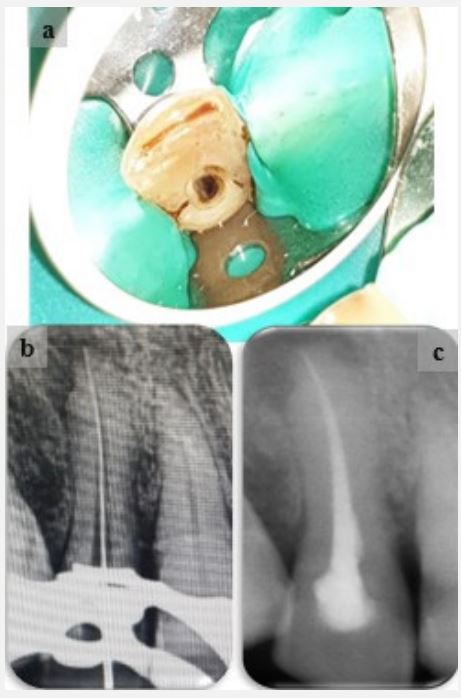
Even in the absence of subjective symptoms, a pulp sensitivity test was conducted, yielding a negative response on tooth 12, indicating pulp necrosis, and a delayed positive response on tooth 22, suggesting chronic pulpitis. To confirm the diagnosis of dens invaginatus, determine its type, and localize it, retroalveolar radiographs were necessary. Regarding tooth 12 (Figure 3a), the invagination presents as an irregular radiopaque outline confined to the cervical third of the tooth crown, not extending beyond the enamel-cementum junction. According to ‘OEHLERS’ classification, this corresponds to dens in dente Type I. The presence of a radiolucent periapical image attached to the tooth’s apex confirms the diagnosis of pulp necrosis and suggests chronic apical periodontitis. As for tooth 22, it exhibits dens in dente Type II characterized by a round and irregularly contoured radiopaque image starting from the cervical third of the tooth crown and extending beyond the enamel-cementum junction, completely obscuring the pulp chamber (Figure 3b).”
a) Periapical Radiograph of Tooth (12):
‑ In blue: Type I dental invagination having appearance of an irregular radio-opaque band confined to the cervical third of the tooth’s crown, not extending beyond the enamel-cementum junction.
‑ In black: Wide root canal.
‑ In red: Radiolucent periapical image suggestive of chronic apical periodontitis. b) Periapical Radiograph of Tooth (22):
‑ In blue: Type II dental invagination having appearance of a rounded, irregularly contoured radio-opaque image starting from the cervical third of the tooth’s crown and extending beyond the enamel-cementum junction, completely masking the cameral pulp.
‑ In black: Narrowed canal lumen.
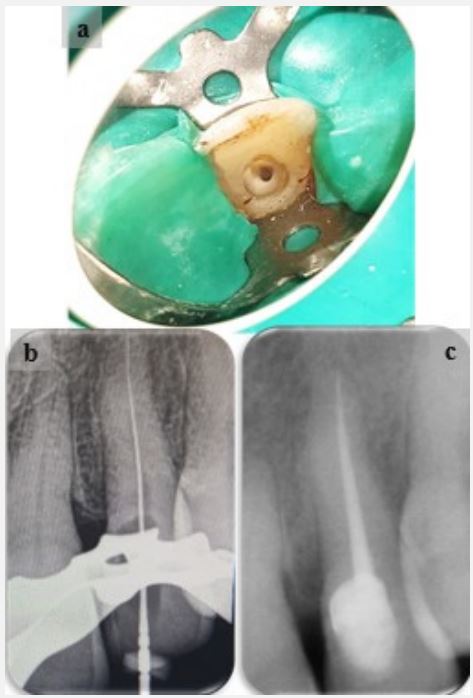
Our management took into account the pulpal involvement and the type of dens invaginatus. Endodontic treatment was indicated for both lateral incisors. For tooth 12, as the structural defect was minimal, the invagination was incorporated into the access cavity and removed during conventional drilling. No bleeding was observed during this procedure, confirming the diagnosis of pulp necrosis (Figure 4a). Once the invagination was removed, canal shaping and cleaning was performed with 2.5% sodium hypochlorite endodontic irrigation, determination of working length (Figure 4b), and a temporary medicated dressing with calcium hydroxide was placed to promote canal disinfection. After two weeks, canal filling was performed using lateral condensation technique (Figure 4c), and finally, the tooth was coronally restored with composite resin.
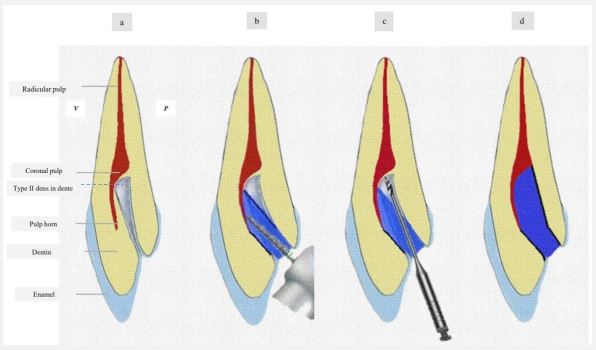
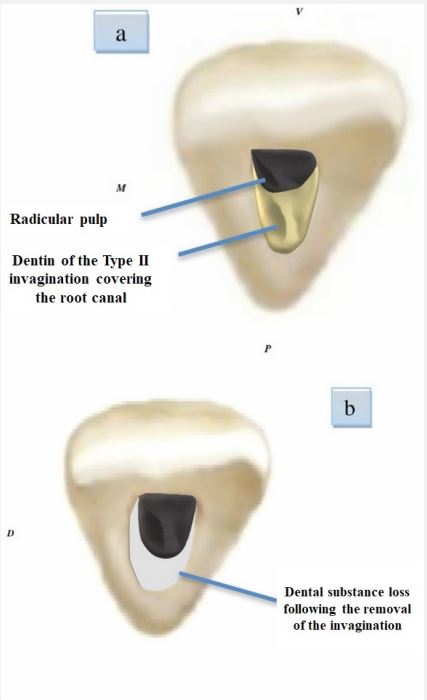
[a]: Initial state: Schematic representation of Type II invagination.
[b]: Beginning of access cavity preparation by removing the coronal portion of dental invagination up to the enamelcementum junction using a round-tipped diamond cylindroconical bur, directed towards the pulp horn.
[c]: Removal of the remaining dental invagination beyond the enamel-cementum junction using a Gates drill #4 in the direction of the root canal, along an axis parallel to the coronoradicular axis of the tooth.
[d]: Schematic representation of the final access cavity.
[a]: Access cavity before the removal of dental invagination, which obstructs access to root canal.
[b]: Access cavity after the removal of dental invagination, providing access to the entire canal system but leaving a significant loss of dental substance.
For tooth 22, where the invagination was deeper, accessing the root canal posed a challenge during treatment. This required a modification in the preparation technique, using a rounded diamond-tipped cylindro-conical bur and a Gates drill #4 to completely remove the hard tissue of the invagination beyond the enamel-cementum junction while ensuring that we stayed within the coronoradicular axis of the tooth (Figure 5). Minimal bleeding was detected during this procedure, confirming the diagnosis of chronic pulpitis. Subsequently, canal instrumentation was performed associated with 2.5% sodium hypochlorite endodontic irrigation (Figure 6a), determination of working length (Figure 6b), and canal filling using the same technique (Figure 6c).
To restore the loss of dental substance caused by drilling in the cervical area (Figure 7), a dental substitute (Biodentine) was placed. This is a bioactive material with compressive strength similar to dentin, which helps reinforce this fragile area and prevent long-term tooth fracture. The treatment was completed with a coronal sealing restoration using composite resin.
Discussion
Dens invaginatus is not a rare clinical finding; it is more common than other developmental anomalies. Its incidence is estimated to be around 2 to 3% [1]. The most commonly affected teeth are the maxillary lateral incisors, and bilateral occurrence occurs in 43% of cases [5], as in our case. Several classifications have been proposed to describe this anomaly, but the “OEHLERS” classification (1957) has gained prominence due to its simplicity and ease of application. The author categorizes invaginations based on radiographic examination into three classes according to their extent from the crown to the root.
Using this classification, the prevalence of dens in dente is 79% for Type I, as tooth 12 in our case, 15% for Type II, as tooth 22, and 5% for Type III. In his studies, “OEHLERS” relied on twodimensional radiographic imaging, as in our case, which could underestimate the extent and complexity of the invagination [4] ; two crucial parameters for diagnosis and treatment planning. In addition to the clinical examination, which can reveal dilated crown morphology, peg-shaped form [5], or, as described in our case, a tubercle shape with a deep cingulum, radiological examination plays a significant role; it determines the type and extent of the invagination, the periapical condition, and potential connections with the pulp and periodontium [1]. Nowadays, new imaging modalities such as CBCT, in contrast to two-dimensional radiography, allow visualization of three-dimensional morphology of the anomaly and provide essential details such as the exact site of emergence and extension of the invagination, its depth, and whether it is associated with apical pathology [6], all with a lower radiation dose, high-resolution images, and time savings [7,8]. Nevertheless, its use remains limited to complex cases. Since the canal system in teeth affected by Type I invagination is relatively simple, the use of CBCT has not been reported to date, and only four studies have been reported in cases of Type II dental invagination [7,3].
The morphological alterations associated with this anomaly can lead to pulp involvement. This was explained by ‘Kramer,’ who observed that a thin layer of dentin at the base of the invagination was not protected by enamel and was exposed to the oral environment, providing a direct pathway into the pulp through the invaginated dentin, potentially allowing bacteria to enter. This supports the concept that even if dens invaginatus may appear small, not communicating with the pulp, and free from caries, it can still lead to pulp necrosis [9].
Pulpal involvement in these cases is sometimes misdiagnosed. ‘Domenico Ricucci and colleagues’ describe a challenging diagnosis situation where the patient complained about pain associated with clinically healthy tooth. After extraction and histological examination Type II dens in dente was discovered, and it is believed to be the cause of pulp necrosis [10]. In our case, the pulp condition of both incisors was assessed using cold test with ethyl chloride and confirmed in-situ while root canal treatment. According to studies, the use of laser Doppler improves the diagnosis accuracy of invaginated teeth. It is a non-invasive, objective, and painless test, but it has limitations such as equipment cost, interference from noise, and movement near or within the device itself [11].
The establishment of a precise pulp diagnosis is essential for treatment plan, which in turn presents challenges due to the internal morphological changes associated with the invagination. Indeed, when endodontic treatment is required, the chemomechanical cleaning and filling of these malformations and the canal system may necessitate various techniques with specific instruments [1,12]. It is advisable to begin by removing the invagination, creating an accessible canal for thorough disinfection and three-dimensional sealing obturation [1].
In the past, ‘Lindner and al.’ believed that the removal of this anatomical obstacle was impossible; however, ‘Girsch & McClammy’ concluded that technological progress has made this therapy possible [13]. In our case, the elimination of Type I invagination on tooth 12 was straightforward using a tungsten carbide cylindrical bur during the access cavity preparation. However, Type II invagination on tooth 22 required a diamondtipped cylindro-conical bur and a Gates drill #4 capable of penetrating beyond the enamel-cementum junction. According to some studies, the ideal approach would involve the use of a long-necked round bur [14]. Additionally, the use of ultrasonic inserts appears to be the ideal instrument in managing these cases [12]. Indeed, the removal of such an entity by ultrasonics is a technique sensitive to the size, location, and accessibility of this structure [15]. Furthermore, the use of an endodontic microscope increases the success rate of the treatment [15].
Locating the canal system in invaginated teeth is a challenging during endodontic treatment, and the risks of weakening the tooth and causing perforations or fractures are not to be overlooked. Therefore, it is essential to consider a procedure capable of locating the access cavity and the canal while preserving maximum dental substance [14,16]. Conventionally, a radiographic examination can be performed to assess the preparation axis and the removal of the invagination [12,13,15]. However, ‘Macho and al.’ proposed a technique using guided implant placement software and splint guides manufactured using stereolithography, but this method can be inaccurate at times, costly, and time-consuming [3,17].
Once the invagination has been removed, conventional endodontic treatment is performed. Sodium hypochlorite endodontic irrigation is essential, and its activation through ultrasonics significantly improves the disinfection of the complex canal system in invaginated teeth [1]. For canal obturation, thermoplastic techniques and the use of bioceramic cements are more recommended [1,7].
Conclusion
Dens invaginatus is a clinically significant dental developmental anomaly due to potential pulp involvement and the development of necrosis. Historically, non-surgical treatment of the root canal in these teeth was considered unrealistic. However, modern endodontics, with the advent of new diagnostic and preparation techniques using specific tools, has overcome the challenges associated with the complex internal anatomy of invaginated teeth and has allowed their successful treatment.
References
- Baumgart M, Hänni S, Suter Beat, Schaffner M, Lussi A. Dent invaginée (densinvaginatus) Revue de la littérature – recommandations diagnostiques et thérapeutiques. Rev Mens Suisse Odontostomatol. 2009 ;7(119): 706-714.
- Achabi N, Hakima C, Hind R. Clinical Guideline for Diagnosis and Treatment of Dens Invaginatus. Integrative Journal of Medical Sciences. 202; 8.
- Zubizarreta Macho Á, Ferreiroa A, Rico-Romano C, Alonso-Ezpeleta LÓ, Mena-Álvarez J. Diagnosis and endodontic treatment of type II dens invaginatus by using cone-beam computed tomography and splint guides for cavity access: a case report. J Am Dent Assoc. 2015; 146(4): 266-70.
- Alani A, Bishop K. Dens invaginatus. Part 1: classification, prevalence and aetiology. Int Endod J. 2008; 41(12): 1123-36.
- Hülsmann M. Dens invaginatus: aetiology, classification, prevalence, diagnosis, and treatment considerations. Int Endod J. 1997; 30(2): 79-90.
- Alkadi M, Almohareb R, Mansour S, Mehanny M, Alsadhan R. Assessment of dens invaginatus and its characteristics in maxillary anterior teeth using cone-beam computed tomography. Sci Rep. 2021; 11(1): 19727.
- Zhu J, Wang X, Fang Y, Von den Hoff JW, Meng L. An update on the diagnosis and treatment of dens invaginatus. Aust Dent J. 2017; 62(3): 261-275.
- Patel S. The use of cone beam computed tomography in the conservative management of dens invaginatus: a case report. Int Endod J. 2010; 43(8): 707-13.
- Hovland EJ, Block RM. Nonrecognition and subsequent endodontic treatment of dens invaginatus. J Endod. 1977; 3(9): 360-2.
- Ricucci D, Milovidova I, Siqueira JF Jr. Unusual Location of Dens Invaginatus Causing a Difficult-to-Diagnose Pulpal Involvement. J Endod. 2020; 46(10): 1522-1529.
- Lee HN, Yan DY, Huang CY, Chen SC, Pan CY, Jeng JH, Chen YK, Chuang FH. Laser Doppler for Accurate Diagnosis of Oehler’s Type III Dens Invaginatus: A Case Report. Applied Sciences. 2021; 11(9): 3848.
- Gallacher A, Ali R, Bhakta S. Dens invaginatus: diagnosis and management strategies. Br Dent J. 2016; 221(7): 383-387.
- Sathorn C, Parashos P. Contemporary treatment of class II dens invaginatus. Int Endod J. 2007; 40(4): 308-16.
- Zubizarreta-Macho Á, Ferreiroa A, Agustín-Panadero R, RicoRomano C, Lobo-Galindo AB, Mena-Álvarez J. Endodontic retreatment and restorative treatment of a dens invaginatus type II through new technologies. J Clin Exp Dent. 2019; 11(6): 570-576.
- Girsch WJ, McClammy TV. Microscopic Removal of Dens Invaginatus. Journal of Endodontics. 2002; 28(4): 336-339.
- Zoya A, Ali S, Alam S, Tewari RK, Mishra SK, Kumar A, Andrabi SM. Double Dens Invaginatus with Multiple Canals in a Maxillary Central Incisor: Retreatment and Managing Complications. J Endod. 2015; 41(11): 1927-32.
- Mena-Álvarez J, Rico-Romano C, Lobo-Galindo AB, ZubizarretaMacho Á. Endodontic treatment of dens evaginatus by performing a splint guided access cavity. J Esthet Restor Dent. 2017; 29(6): 396-402.