Research Article
Volume 3, Issue 2
Comparison of Honey Wax and Olive Oil with 1% Silver Sulfadiazine Dressing on Pain and Wound Healing in Burn
Arezou Karampourian1; Javad Feradmal2; Roya Amini3*; Shirin Moradkhani4; Mohammad Yousef Alikhani5 ; Rasoul Salimi6; Nahid Mohammadi7
1Assistant Professor, Urology and Nephrology Research Center, Chronic Diseases (Home Care) Research Center, School of Nursing and Midwifery, Hamadan University of Medical Sciences, Hamadan, Iran.
2Professor of Biostatistics, Department of Biostatistics, School of Health, Modeling of Noncommunicable Diseases Research Center, Health Sciences & Technology Research Institute, Hamadan University of Medical Sciences, Hamadan, Iran.
3nstructor of Community Health Nursing, Department of Community Health Nursing, School of Nursing and Midwifery, Chronic Diseases (Homecare) Research Center, Hamadan University of Medical Sciences, Hamadan, Iran.
4Associate Professor of Pharmacognosy, Department of Pharmacognosy, School of Pharmacy, Medicinal Plants and Natural Products Research Center, Hamadan University of Medical Sciences, Hamadan, Iran.
5Professor of Medical Bacteriology, Department of Microbiology, School of Medicine, Brucellosis Research Center, Hamadan University of Medical Sciences, Hamadan, Iran.
6Assistant Professor of Emergency Medicine, Department of Emergency Medicine, School of Medicine, Hamadan University of Medical Sciences, Hamadan, Iran.
7nstructor of Community Health Nursing, Department of Community Health Nursing, School of Nursing and Midwifery, Chronic Diseases (Homecare) Research Center, Hamadan University of Medical Sciences, Hamadan, Iran.
Corresponding Author :
Roya Amini
Tel: + 98-918-315-2273;
Email: amini@umsha.ac.ir
Received : Dec 14, 2023 Accepted : Jan 26, 2024 Published : Feb 02, 2024 Archived : www.meddiscoveries.org
Citation: Karampourian A, Feradmal J, Amini R, Moradkhani S, Yousef Alikhani M, et al. Comparison of Honey Wax and Olive Oil with 1% Silver Sulfadiazine Dressing on Pain and Wound Healing in Burn. Med Discoveries. 2024; 3(2): 1111.
Copyright: © 2024 Amini R. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Background: Burn is painful, and burn wound healing is a prolonged process. This study aimed to compare the effects of Honey Wax and Olive oil with 1% Silver Sulfadiazine (SSD) dressing on burn wound pain attenuation and healing.
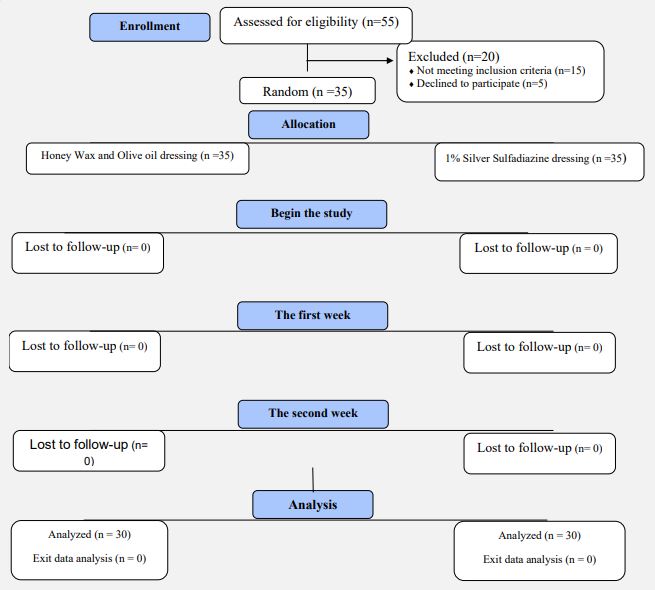
Methods: Patients with two burn wounds were randomly divided into two groups. One group was dressed with honey wax and olive oil (intervention) and another wound was dressed with SSD (control). The instruments included the Burn Wound Healing Checklist, Demographic and Clinical questionnaire, and Visual Analogue Scale. Data were analyzed using independent t-test and repeated measures analysis of variance tests in SPSS 23 software.
Results: There was a significant difference between the intervention group (10.28±1.15 days), and the control group (14.77±1.77 days) in terms of healing duration. On the baseline, healing and pain were not different in the two groups; however, there was a significant difference between the two groups over time. From baseline to day 7 and from day 7 to 14, wound healing improved in the intervention group compared to the control group. Moreover, from day 7 to day 14, the mean pain intensity attenuated in the intervention group compared with the control group.
Conclusion: It is recommended to use this combination for dressing burn wounds in non-hospitalized partial thickness burn patients with TBSA≤15%.
Keywords: Burns; Pain; Wound Healing; Silver Sulfadiazine; Complementary Therapies.
Background
An increase in accidents is among the most important dangers that threaten human life [1,2]. Accident injuries were the second leading cause of disability in developing countries by 2020, and the third leading cause of death and disability worldwide [3]. One of the major accidents is burns. In fact, burns are a global public health problem and cause 180,000 deaths annually. Most burns occur in low- and middle-income countries, and about two-thirds of them occur in Africa and Southeast Asia [4]. In addition to incurring high costs on the individual and society, burns also cause disability [5,6]. Burn patients face a number of physical, psychological, and functional complications. Prolonged hospitalization, deformity and disability reduce the quality of life of patients [7-9]. Burn wound care is one of the most important duties of a nurse. Pain has been identified by nurses as one of the major problems with wound dressing change [10]. Various dressings can be applied to heal burn wounds. Burn dressings should have the following characteristics: resistance to microorganisms, penetration into the scar tissue, cost-effectiveness, acceptability, ease of use, and no need for frequent replacement [10]. Currently, one of the most common burn dressings is silver sulfadiazine (SSD). SSD has several side effects, such as lack of penetration into the wound, resistance to negative microorganisms, and delayed wound healing [11]. Various studies have shown that dressing with a combination of traditional medicines like honey in the treatment of wounds and burns is cost-effective and reduces the healing duration and complications as well [12,13]. Honey has antimicrobial, antioxidant, and anti-inflammatory properties due to its compounds, such as sugar, minerals, proteins, vitamins, acids and antioxidants. It is used in commercial products as a prebiotic, wound healing agent, and food preservative [14,15]. Honey is more effective in treating superficial and partial burns and in reducing infection risk as compared with other therapies, such as SSD. Other advantages of honey include being cheap, non-toxic and non-allergenic, non-stick to the wound site, providing a moist environment, and reducing pain when changing dressings [16,17]. A systematic review study of nine clinical trials found that using a honey dressing compared to SSD ointment could reduce the duration of burn wound healing. In addition, it prevents wound infection risk [13]. The results of a systematic review study also showed that the use of honey in burns causes rapid epithelialization in wound healing, leads to anti-inflammatory and debilitating effects, and reduces pain [18]. Besides honey, olive oil also has antioxidant, anti-inflammatory, and antibacterial properties and can affect wound healing [19,20]. As limited research has been done on the effect of honey and olive oil combination on burn wound healing, the researchers decided to conduct a study to compare the effects of using olive oil + honey wax dressing with 1% SSD on burn wound healing and pain attenuation.
Materials & methods
Design: This clinical trial was conducted on partial thickness (second-degree) burn patients with two burn wounds in an outpatient clinic in 2022.
Sampling method: The sample size was calculated 35 based on Imani’s study and using the following formula (11).
n= (z1-α/2+z1-β) 2σ2/ d 2
Patients with two burn wounds were randomly divided into two groups. The wounds were the same in terms of depth, in fact, they were all superficial 2nd degree burns, but they were different in terms of extent. In total, the width of the wounds was considered 15%, because the width more than this will be admitted to the hospital, which was not considered by the authors.
The inclusion criteria: Patients with two wounds, burn with 15% extentmaximum, age range of 5-60 years, burn in areas except head, neck, and perineum, time from burn to sampling of less than 6-8 hours, no other diseases such as malnutrition, anemia, diabetes, skin allergies, malignancy, no cytotoxic drugs, no chemical or electrical burns, and with no use of any substance other than water on the wound at the time of admission.
The exclusion criteria: Purulent discharge, swelling, discoloration, sensitivity, fever, and the patient’s refusal for dressing change.
Method
In the intervention group, the dressing was performed with honey wax and olive oil, however, in the control group, dressing was performed with 1% SSD ointment. In both groups, the wound was dressed sterilely. In the presence of necrotic tissue, the wound was the first debridement and then dressed with a combination of honey wax and olive oil or 1% SSD ointment. In the intervention group, the dressing was changed every other day for three weeks however, in the control group was done every day. To check the condition of the burn wound, the burn wound healing checklist was used after each dressing change. The presence of a thin, clear, pink membrane with no discharge and no covering tissue was considered a sign of wound healing and the dressing change process was stopped.
The method of making the composition honey wax and olive oil: The combination was prepared as follows: 600 g of olive oil and 1000 g of multi-floral honey wax were mixed together at a temperature above 100°C to form a semi-solid soft compound. This compound was examined before use in the microbiology laboratory and sterilized for three days using a tendalization method at a temperature of 80°C for 30 minutes every day for three days. For three consecutive days, the compound was heated at first for half an hour and then reached 37°C to prevent spore growth.
Research instrument: The research instruments included the Burn Wound Healing Checklist, Demographic and Clinical Questionnaire, and Visual Analogue Scale (VAS). The Burn Wound Healing Checklist criteria included the amount of wound discharge, color of wound discharge, wound odor, necrotic tissue, color of tissue surrounding the wound, and wound condition in terms of granulation and epithelial tissue. The minimum and maximum score obtained in this checklist was 6 and 24, respectively.
The Demographic and Clinical questionnaire asked about age, gender, education, place of residence, time from burn onset, measures taken from time of burn to outpatient clinic, cause of burn, estimation of burn surface (TBSA), burn area, and history of underlying conditions and medication use.
Visual Analogue Scale (VAS) was used to measure pain intensity during dressing. The criterion for pain intensity is from zero to ten. VAS consists of a 10-centimeter line with 0 representing no pain, 1-2 mild pain, 3-5 moderate pain, 7-9 severe pain and 10 unbearable pain.
The validity of the burn wound healing checklist was examined in a study by Imani et al. and the reliability of the instrument was found to be 0.9 [11]. The validity and reliability of pain intensity measuring instruments (VAS) were confirmed in similar studies [20]. Data were analyzed using an independent ttest and repeated-measures analysis of variance (ANOVA) with the SPSS 23.0 software.
Results
The results showed that most of the patients in this study were female (60%), the mean age of the patients was 47.40±18.57, and the diploma was (57.14%). In most patients, hot liquids were the cause of burn (65.71%), upper extremities were the most frequent anatomical burn sites (60%), and time from burn to referral was 4-6 hours (60%) (Table 1).
Total body surface area: In most wounds treated with honey wax and olive oil, the wound healed within 7-10 days; however, in most wounds treated with 1% SSD, the healing duration was 11-14 days. Fisher’s exact test showed a significant difference in different categories of healing time between the two wound groups (P=0.003). The average duration of healing in patients treated with honey wax and olive oil dressing was 10.28±1.15 days, and 14.77±1.77 days in those treated with 1% SSD. The results of independent t-test showed that there was a statistically significant difference between the two wound groups in terms of woud healing duration (P<0.001) (Table 2).
Independent t-test: There was no statistically significant difference in terms of mean score of total wound healing and its dimentions, namely wound discharge, wound discharge color, wound odor, necrosis tissue, wound granulation tissue in the two wound groups at the baseline (P>0.05); however, In the first week of the study, there was a statistically significant difference in terms of mean score of all dimentions of woud healing except for color score of tissue surrounding wound (P=0.095). Furthermore, in the second week of the study, there was a statistically significant difference in the mean score of total wound healing and its dimentions between the two groups (P<0.05) (Table 3).
Table 1: Demographic data.
| Variables | ||
|---|---|---|
| Age, M ± SD | 47.40±18.57 | |
| Gender, n (%) | Female | 21 (60.00) |
| Male | 14 (40.00) | |
| Education level | Reading & Writing | 3 (8.57) |
| High school | 10 (28.57) | |
| Diploma | 20 (57.14) | |
| Accademic | 2 (5.72) | |
| Burn etiology | Fire flame | 7 (20.00) |
| Hot liquids | 23 (65.71) | |
| Hot objects | 5 (14.28) | |
| Burn location | Upper limb | 21(60.00) |
| Lower limb | 11 (31.43) | |
| Thrunk | 3(8.57) | |
| Burn time to referral (hours) | 3 and less | 8 (22.86) |
| 4 - 6 | 21 (60.00) | |
| 7 - 8 | 6 (17.14) | |
Table 2: Comparison of burn wound healing duration in two dressing groups
| Combination | Burn healing time (days) | Statistical test╟ |
|---|---|---|
| Mean ± SD | ||
| Honey wax and olive oil | 10.28±1.15 | t=16.5 p<0.001 |
| Silver sulfadiazine 1% | 14.77±1.11 |
Table 3: Comparison of mean scores of burn wound healing dimensions in the two groups of patients’ wound.
| Woud healing | Wound group | Baseline Mean ± SD | Day 7 Mean ± SD | Day 14 Mean ± SD |
|---|---|---|---|---|
| Wound discharge | Silver sulfadiazine 1% | 1.43±.5 | 2.17±.38 | 2.34±.59 |
| Honey wax and olive oil | 1.66±.48 | 2.46±.50 | 3.23±.73 | |
| p value ╟ | P=.061 | P=.010 | P<.001 | |
| Wound discharge color |
Silver sulfadiazine 1% | 1.88±.32 | 2.14±.35 | 2.48±.66 |
| Honey wax and olive oil | 1.86±.35 | 2.40±.50 | 3.23±.73 | |
| p value ╟ | P=.726 | P=.015 | P<.001 | |
| Wound discharge odor | Silver sulfadiazine 1% | 2.11±.32 | 3.00±.00 | 3.08±.28 |
| Honey wax and olive oil | 2.14±.35 | 3.14±.35 | 3.31±.47 | |
| p value ╟ | P=.726 | P=.020 | P=.017 | |
| Necrosis tissue | Silver sulfadiazine 1% | 3.34±.48 | 3.46±.50 | 3.54±.50 |
| Honey wax and olive oil | 3.43±.50 | 3.77±.43 | 3.86±.35 | |
| p value ╟ | P=.469 | P=.006 | P=.004 | |
| Tissue color around the wound | Silver sulfadiazine 1% | 3.03±.62 | 3.34±.48 | 3.48±.51 |
| Honey wax and olive oil | 3.14±.65 | 3.54±.50 | 3.77±.43 | |
| p value ╟ | P=.453 | P=.095 | P=.013 | |
| Wound granulation tissue | Silver sulfadiazine 1% | 2.40±.50 | 3.06±.42 | 3.60±.50 |
| Honey wax and olive oil | 2.60±.55 | 3.31±.47 | 3.86±.35 | |
| p value ╟ | P=.116 | P=.018 | P=.015 | |
| Total | Silver sulfadiazine 1% | 14.32±1.08 | 17.17±1.22 | 18.54±1.44 |
| Honey wax and olive oil | 14.83±1.17 | 18.63±1.50 | 21.26±1.88 | |
| p value ╟ | P=.064 | P<.001 | P<.001 |
Independent t-test.
Table 4: Comparison of honey wax and olive oil dressing with silver sulfadiazine 1% dressing in wound healing (day).
| Wound healing (day) | Base line | Day 7 | Day 14 | Statistical tests |
|---|---|---|---|---|
| Honey wax and olive oil | 14.83±1.17 | 18.63±1.50 | 21.26±1.88 |
F=15.86 p╟╟< .001 |
| Silver sulfadiazine 1% (1% SSD) | 14.32±1.08 | 17.17±1.22 | 18.54±1.44 | |
| t=-1.88 p╟=.064 |
t=-4.46 p╟<.001 |
t=-6.77 p╟<.001 |
Independent t-test: Repeated measures ANOVA.
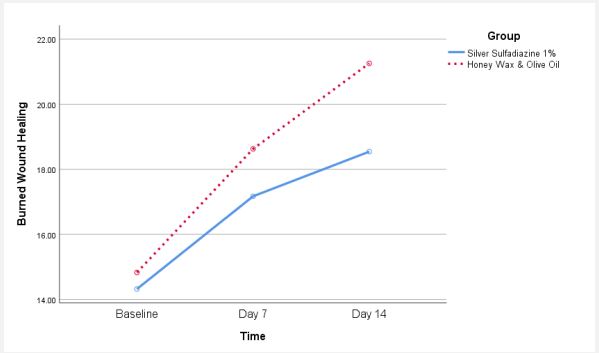
On the baseline, the mean wound healing rate was not different between patients’ wounds dressed with honey wax and olive oil and 1% SSD dressing (P=0.064); however, there was a significant difference in terms of wound healing on day 7 (P< .001) and day 14 (P < 0.001) between two groups of wounds. Moreover, the two-way repeated measures ANOVA showed a significant difference in the mean scores on patients’ wound healing between the two groups of wounds over time (P<0.001) (Table 4).
Furtheremore, the effect of the honey wax and olive oil mixture and 1% SSD dressing on wound healing over time is illustrated in Figure 1. Post hoc tests showed that from baseline to day 7, the mean wound healing improved in patients’ wounds dressed with honey wax and olive oil mixture as compared with 1% SSD (P=.004, F=8.78), and from day 7 to 14, the mean wound healing also improved in honey wax and olive oil dressing compared to 1% SSD dressing (P=0.002, F=10.54) (Figure 1).
The Post hoc tests showed that from baseline to day 7, the mean pain intensity was the same in patients’ wounds dressed with honey wax and olive oil mixture in comparison to 1% SSD (P=.145, F=2.17), and from day 7 to day 14, the mean pain intensity attenuated in patients’ wounds dressed with honey wax and olive oil as compared with 1% SSD (P=0.001, F=13.07) (Figure 2).
Table 5: Comparison of honey wax and olive oil dressing with 1% SSD dressing in pain intensity of burn patients.
| Wound healing (day) | Base line | Day 7 | Day 14 | Statistical tests |
|---|---|---|---|---|
| Honey wax and olive oil | 5.43±1.19 | 1.68±.72 | .48±.56 | F=8.99 P=.001 |
| Silver sulfadiazine 1% (1% SSD) | 5.34±1.39 | 2.11±.67 | 1.68±.58 | |
| t=-.28 p=.783 |
t=2.57 p=.012 |
t=-8.76 p<.001 |
Independent t-test: Repeated measures.
Discussion
The results of the present study showed that the combination of honey wax and olive oil can reduce the healing duration of partial thickness burns and also attenuate pain during dressing.
Yilmaz’s study showed that dressing a burn wound with honey caused less wound inflammation than with muffin acetate. It also accelerated the epithelialization process. In addition, side effects such as pigmentation and scarring were rare in dressing with honey. It was thus suggested that honey be used as a wound dressing [18]. Liche’s study showed that the mean healing time of burn wounds in the pediatric age group treated with honey dressing (11±4) was faster than in those treated with silver dressing (15±6). The results of this study showed that dressing with honey has a significant effect on reducing infection risk and on healing burn wounds in children [22]. The results from Azman’s clinical trial study also showed that the duration of burn wound healing in children in the honey dressing group was shorter than the plain foam dressing group [23]. Saeidinia compared SSD with the herbal drug (an herbal compound derived from Centella asiatica). The results showed that Centiderm outperformed SSD in terms of burn wound healing, and the average time of re-epithelialization of burn wound dressing with Centiderm was about one week less than that of SSD [24]. In fact, the high acidity and osmolarity of honey limit the activity of protease enzyme. Restriction of enzymatic activity improves the wound healing process. Honey has numerous biological activities that encourage the immune response, prevent inflammation, and also remove dead tissue. This increases the wound healing process [25]. Olive oil also has antioxidant and anti-inflammatory properties [19]. Phenolic compounds in olive oil have a biostimulatory effect on regeneration and lead to the differentiation and migration of fibroblasts. In addition, it has antibacterial and strong therapeutic effects on wound healing [20].
The results of the present study showed that the mean pain score during dressing with honey wax and olive oil was similar to dressing with SSD at the beginning of the study; however, seven and fourteen days after the burn, the mean pain intensity of dressing with honey wax and olive oil was significantly lower than dressing with SSD. This means that the mean pain score in dressing with honey wax and olive oil was lower than dressing with SSD (P=0.001). The results obtained from a study by Harsono showed that dressing burns with honey compared to MEBO ointment, a traditional ointment used in Indonesia, further reduces the average pain score during dressing [26]. The results from Saeidinia’s study showed that the mean pain score during burn dressing on the third, seventh and fourteenth days in the SSD group was higher than in the Centiderm group [24]. In a study, Bokaiean et al. In a study, Bokaiean et al. made a comparison between manuka honey dressing and conventional dressing with regard to skin graft donor sites after a burn injury. The results of their study showed that the mean pain score was lower in the honey group than in the conventional dressing group, and there was a significant difference between the two wound sites in terms of mean pain score [27]. In general, the results of most studies showed that dressing a burn wound with honey was more effective than other dressings used for pain attenuation during dressing. Honey is suitable for dressing burn wounds. In fact, honey can help remove dead tissue more easily by creating a moist environment, and thus reduce pain during dressing. Moreover, honey may act on anti-inflammatory and immune-mediated mediators leading to pain control. This mechanism can occur in the central and peripheral nervous system or autonomic receptors. Furtheremore honey can affect the cyclooxygenase pathway [17].
Limitation: Individual, cultural, social, and economic differences are among the factors influencing burn wound healing that cannot be controlled and are considered limitations of the study.
Conclusion
The results from this study also showed that the combination of olive oil and honey wax dressing is more effective than 1% SSD dressing on pain and healing wounds in the burn. It is thus recommended to use this combination for dressing burn wounds in non-hospitalized patients with partial thickness burns and TBSA≤15%.
Declarations
Ethics approval and consent to participate: The study protocol was approved by the Ethics Committee with the number 960212932. The IRCT code was IRCT2016071325846N2. Written consent was obtained from all patients.
Conflict of interest: There is no conflict of interest by the authors.
References
- Moradi A, Rahmani K. Trend of traffic accidents and fatalities in Iran over 20 years (1993-2013). Journal of Mazandaran University of Medical Sciences. 2014; 24(119): 223-34.
- Park’s K, K P. Park’s Text Book of Preventive and Social Medicine. 11 ed: MIIM Digital library E -Books. 2021.
- Maraci M, Tabaresfahani M. The burden of road traffic injuries in Isfahan, Iran in 2010. Journal of Kerman University of Medical Sciences. 2013; 20(5): 505-19.
- Organization WH. Burns. 2018. https://www.who.int/newsroom/fact-sheets/detail/burns.
- Mobayen M, Ghaffari ME, Shahriari F, Gholamrezaie S, Dogahe ZH, Chakari-Khiavi A. The epidemiology and outcome of burn injuries in Iran: A ten-year systematic review and meta-analysis. 2021.
- Abbasi H, Dehghani A, Mohammadi AA, Ghadimi T, Keshavarzi A. The Epidemiology of Chemical Burns Among the Patients Referred to Burn Centers in Shiraz, Southern Iran. Bulletin of Emergency And Trauma. 2021; 2008-2018.
- Chen L, He X, Xian J, Liao J, Chen X, Luo Y, et al. Development of a framework for managing severe burns through a 17-year retrospective analysis of burn epidemiology and outcomes. Scientific reports. 2021; 11(1): 1-11.
- Chin TL, Carrougher GJ, Amtmann D, McMullen K, Herndon DN, Holavanahalli R, et al. Trends 10 years after burn injury: a burn model system national database study. Burns. 2018; 44(8): 1882-6.
- McAleavey AA, Wyka K, Peskin M, Difede J. Physical, functional, and psychosocial recovery from burn injury are related and their relationship changes over time: A Burn Model System study. Burns. 2018; 44(4): 793-9.
- Janice L Hinkle, Cheever KH. Brunner & Suddarth’s Textbook of Medical-Surgical Nursing. 14 ed: Lippincott. 2018.
- Imani b, Kermanshahi S, Moosavi K. To compare effect of hydrocolloid dressing and 1% silver sulfadiazine dressing on burn status wounds in patients with second-degree burn. Daneshvar medicine. 2010; 16(84): 63-70.
- Diamond A, Bowler M. Honey Vs. Silver Sulfadiazine in the Reepithelialization of Partial-Thickness Burn Wounds The Graduate School at JMU Scholarly Commons. 2020. https://commons.lib.jmu.edu/pacapstones202029].
- Aziz Z, Hassan BAR. The effects of honey compared to silver sulfadiazine for the treatment of burns: A systematic review of randomized controlled trials. Burns. 2017; 43(1): 50-7.
- Sachdev S, Kumar A, Ansari MI. Health Benefit, Traditional, and Modern Uses of Natural Honey. Non-Timber Forest Products: Springer. 2021: 281-99.
- Al-Waili N, Salom K, Al-Ghamdi A, Ansari MJ. Antibiotic, Pesticide, and Microbial Contaminants of Honey: Human Health Hazards. 2012.
- Almasaudi S. The antibacterial activities of honey. Saudi journal of biological sciences. 2021; 28(4): 2188.
- Lazim N, Baharudin A. Honey-a natural remedy for pain relief. Nutritional Modulators of Pain in the Aging Population: Elsevier. 2017; 123-34.
- Yilmaz AC, Aygin D. Honey dressing in wound treatment: a systematic review. Complementary Therapies in Medicine. 2020; 51: 102388.
- Badiu D, Rajendram R. Effect of olive oil on the skin. Olives and olive oil in health and disease prevention. 2021: 401-13.
- Melguizo-Rodríguez L, Illescas-Montes R, Costela-Ruiz VJ, Ramos-Torrecillas J, de Luna-Bertos E, García-Martínez O, et al. Antimicrobial properties of olive oil phenolic compounds and their regenerative capacity towards fibroblast cells. Journal of Tissue Viability. 2021.
- Ferreira-Valente MA, Pais-Ribeiro JL, Jensen MP. Validity of four pain intensity rating scales. Pain®. 2011; 152(10): 2399-404.
- Liche E, Zulu R, Kasongo Z, Munthali J. Effects of silver sulfadiazine and Actilite® honey on bacteria wound colonisation and wound healing in children with partial superficial burn wounds at University Teaching Hospital, Lusaka, Zambia. Medical Journal of Zambia. 2018; 45(4): 210-5.
- Azman N, Hussein H, Cheng S. Honey dressing versus foam dressing on pediatric burns: Comparison of numbers of burn dressing change. ANZBA 2018http://www.anzbaasm.com/wp-content/uploads/2018/10/Nurazlin-Mohd-azman-ANZBA-ePoster. 2018.
- Saeidinia A, Keihanian F, Lashkari AP, Lahiji HG, Mobayyen M, Heidarzade A, et al. Partial-thickness burn wounds healing by topical treatment: A randomized controlled comparison between silver sulfadiazine and centiderm. Medicine. 2017; 96(9): 6168.
- Oti VB. Wound Healing: Understanding Honey as an Agent. Wound Healing Research: Springer. 2021; 149-76.
- Harsono AD, Wardhana A. Randomized Control Trial Comparing Moist Exposed Burn Ointment and Honey as Dressings Agents in Patients with Second-Degree Burns. Jurnal Plastik Rekonstruksi. 2013; 2(1).
- Bokaiean R, Momeni M, Sabrjoo P, Dahmardehei M, Roham M, Rahber H. Comparing active Leptospermum honey dressing with conventional dressing in skin graft donor sites. Iranian Journal of Dermatology. 2018; 21(1): 1-6.