Case Report
Volume 2, Issue 8
Stent Implantation in One Case of Atherosclerotic Vertebrobasilar Artery Stenosis and Literature
Jing-Gang Bao1#; Feng-Fan Bai2#; Chen He1#; Xiang-Ji Lu1#; Jian-Ping Zhang1#; Gang Yang3; Xin-Wei Zhu1; Xiao-Dong Wang2; Ri-Le Wu1
1Emergency Cerebrovascular Department, Inner Mongolia Autonomous Region People’s Hospital, Hohhot, China.
2Department of Emergency Medicine, Inner Mongolia Armed Police Corps Hospital, Hohhot, China.
3Cardiothoracic Surgery Department, Central Theater Command General Hospital, WuHan 430000, China.
#Contributed Equally to the Present Work.
Corresponding Author :
Wang Xiaodong & Wu Rile
Email: 302758945@qq.com & wurile@hotmail.com
Received : Jul 05, 2023 Accepted : Aug 04, 2023 Published : Aug 11, 2023 Archived : www.meddiscoveries.org
Citation: Jing-Gang B, Feng-Fan B, Chen H, Xiang-Ji L, Ri-Le W, et al. Stent Implantation in One Case of Atherosclerotic Vertebrobasilar Artery Stenosis and Literature. Med Discoveries. 2023; 2(8): 1060.
Copyright: © 2023 Xiaodong W & Rile W. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Intracranial Atheromatous Disease (ICAD) accumulates intracranial large vessels, which is one of the most common causes of ischemic stroke. The risk factors for ICAD include advanced age, smoking, hypertension, hypercholesterolemia and insulin-dependent diabetes mellitus [1-3]. The mechanisms of stroke caused by stenosis of vascular lumen caused by intracranial atherosclerotic disease include: 1) Hypoperfusion; 2) vessel occlusion due to plaque rupture, bleeding or plaque enlargement at the stenotic site resulting in thrombosis; 3) distal embolism caused by thrombus detachment; 4) perforator vessel occlusion at the stenosis site; 5) Combined action of the above mechanisms. The degree of intracranial artery stenosis is related to the risk of ischemic stroke. It has been suggested that the risk of ischemic cerebrovascular disease will increase by 26% for every 10% increase in the degree of intracranial artery stenosis. Chimowitz MI et al. [4] showed that despite standard antiplatelet therapy, patients with symptomatic severe intracranial artery stenosis (stenosis rate of 70%-99%) were followed up for an average of 1.8 years, the recurrence rate of stroke was still more than 22.1%, and the annual incidence of ischemic stroke in the stenosed area was 12%. Sammpris et al. [5] showed that the recurrence rate of stroke in patients with severe intracranial artery stenosis was 12.2% within 1 year under regular medical treatment. Therefore, the FDA restricted the use of stents to patients with 70 to 99% stenosis who had two or more strokes despite medical conservative therapy and who had been stroke free in the previous 7 days. In recent years, with the continuous progress of endovascular treatment methods and the development of materials science, the success rate of intracranial stent treatment is getting higher and higher, which brings new hope for the treatment of intracranial artery stenosis. Balloon angioplasty was the first endovascular revascularization technique used in the intracranial circulation, and Sundt et al. [6] first reported it for the treatment of basilar artery stenosis. The technical success rate of balloon angioplasty is very high (residual stenosis <50%) with a perioperative complication rate of 5.8% to 50% [7]. However, this technique has several disadvantages, including acute elastic retraction of the vessel leading to postoperative residual stenosis, vascular dissection, acute thrombosis, and high rates of restenosis.
Keywords: Atherosclerosis; Ischemic stroke; Vertebral artery stenosis; Stent implantation balloon dilation.
Introduction
Our cerebrovascular intervention team has made active and meaningful exploration in angioplasty and stent implantation of intracranial artery stenosis. Here is a case of intracranial artery stenosis that we recently treated. We selected patients strictly according to the indications of intracranial stenting in the latest guidelines: 1) patients with first or recurrent symptomatic intracranial large artery stenosis who had failed medical treatment; 2) DSA showed that the degree of intracranial stenosis was ≥70%; 3) Imaging examination within 2 weeks before surgery indicated poor collateral circulation in the area of offending vessel disease. In this case, a comprehensive preoperative evaluation was performed to confirm that the patient was within the indications and excluded from the contraindications.
Case presentation
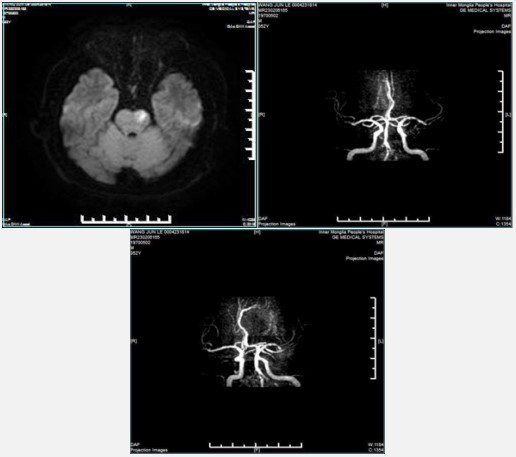
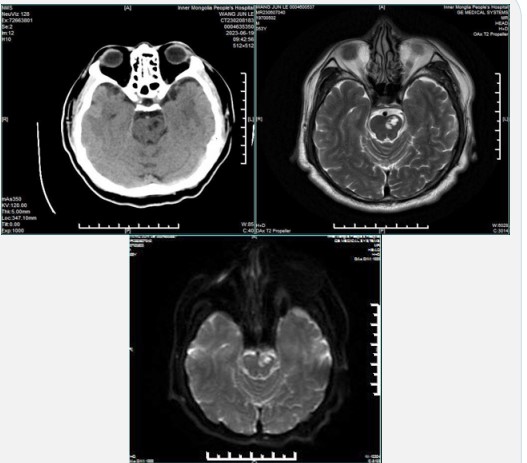
A 53-year-old male patient was admitted to the cerebrovascular department with the chief complaint of dizziness for more than 4 months. The patient was transferred to the neurology ward from the emergency department due to dizziness 4 months ago without obvious precipitating factors and unrelated to body position. MRI showed cerebral infarction, which was improved after conservative medical treatment, and oral aspirin and atorvastatin calcium were continued. Post-specialist outpatient reexamination of head and neck vascular CTA (May 11, 2023) suggested: 1) Multiple calcification, mixed plaque and mild stenosis were found in C3-C6 segment of the left internal carotid artery; 2) The right C6 segment of the internal carotid artery wall punctate calcified plaque, mild lumen stenosis; 3) Left subclavian artery localized non-calcified plaque with mild stenosis; 4) Severe stenosis of the V4 segments of bilateral vertebral arteries; 5) Basilar fenestration malformation. Now for further treatment, the patient was admitted to the Cerebrovascular department as “bilateral vertebral artery stenosis”. Risk factors included: history of hypertension for 10 years, treatment with oral indapaan, type 2 diabetes for 1 year, and treatment with oral metformin and acarbose. The patient denied the history of chronic disease, blood transfusion, drug allergy, trauma and surgery, coronary heart disease, etc. No obvious abnormal signs were found in the admission physical examination.
The patient was admitted to the department of cerebrovascular disease on June 5, and blood glucose and blood pressure were monitored. (5 days before surgery) on June 8, aspirin enteric-coated tablets 100 mg, QD, clopidogrel bisulfate tablets 75 mg, QD, oral atorvastatin calcium tablets 10 mg, QN were given. On June 15, he was given subcutaneous injection of low molecular weight heparin sodium 4250 IU every 12 hours.
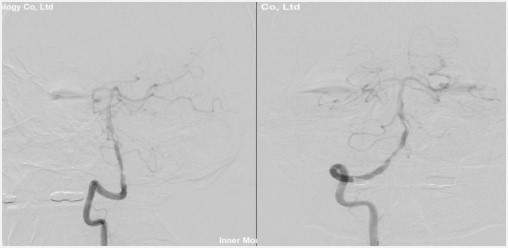
Cerebral arteriography was performed under local anesthesia on June 13, 2023, and the procedure was recorded as follows: The patient was placed in the supine position, and the inguinal area was routinely sterilized and placed with a sheet. After local anesthesia, right femoral artery puncture was performed. A 5F angiographic catheter was inserted, and a 5F single curved angiographic catheter was placed under the guidance of 0.035 in hydrophilic wire for angiography of left and right carotid and vertebral arteries. The results of angiography showed moderate stenosis of the V4 segment of the left vertebral artery, moderate stenosis of the right vertebral opening, severe stenosis of the right vertebrobasilar artery and fenestration malformation, and moderate stenosis of the V4 segment of the right vertebral artery. The angiography was uneventful and the patient complained of no discomfort. At the end of operation, the arterial sheath was removed and compressed for 15 minutes to stop bleeding. Appropriate treatment such as fluid infusion was given after operation.
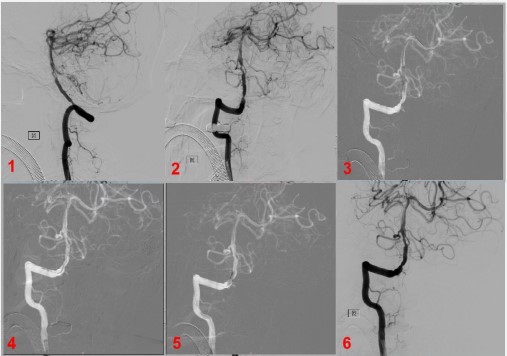
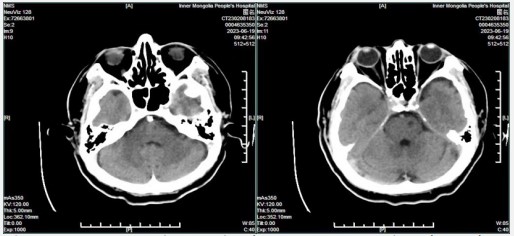
One day later, on June 15, 2023, the patient underwent "balloon dilation and stenting of the basilar artery and V4 balloon dilation of the right vertebral artery" under general anesthesia. The patient was placed in the supine position, routinely sterilized, covered with towels, and right femoral artery puncture was performed. A 6F Catheter sheath was inserted, a 6F Guide Catheter and a 5F multifunctional catheter were sent to the V3 segment of the right vertebral artery, then Y valve and double tee were connected, one tee was connected with contrast agent, one tee was connected with continuous pressure perfusion of heparin saline. The micro-guidewire was sent to the left posterior cerebral artery, and the intracranial PTA Balloon Catheter (2 mm/15 mm) was sent to the right vertebrobasilar artery fenestration deformity and severe stenosis for balloon dilatation. Angiography showed that the vertebrobasilar artery stenosis was significantly improved. After several minutes of observation, angiography showed re-stenosis with slow blood flow. Intracranial PTA Balloon Catheter (2.5 mm/20 mm) was sent to the severe stenosis of the right vertebrobasilar artery for balloon dilatation, and down to the stenosis of the V4 segment of the right vertebral artery for balloon dilatation. Angiography showed that the two vertebrobasilar artery stenosis were significantly improved. After inserting the EXcelsior XT-27 microcatheter (150 cm × 6 cm) into the corresponding position, the Neuroform EZTM 4.0 mm × 20 mm stent was placed in the stenosis segment of the vertebral base to completely cover the stenosis at both ends. After accurate positioning under the roadmap, the catheter was withdrawn and the stent was slowly released under fluoroscopy. The stent adhered well and completely covered the stenosis segment. Angiography showed that the stenosis was significantly improved, the blood flow in the stent was unobstructed, and the branch vessels were well developed. The femoral artery puncture point was sutured and pressure bandaged at the end of operation. After surgery, the patient was awake and extubated with fluent speech and good limb movement. Routine postoperative CT scan was performed to exclude Intracranial Hemorrhage (ICH). The patient was transferred to the neurological intensive care unit and received hemodynamic monitoring with active systemic blood pressure control. Low molecular weight heparin calcium, clopidogrel and aspirin were used to prevent thrombosis. For vertebrobasilar angioplasty and stenting, CTA or DSA should be performed at 3 months, 6 months, and 12 months after surgery.
Discussion
Intracranial Atherosclerotic Stenosis (ICAS) is one of the most common causes of ischemic stroke and one of the risk factors for stroke recurrence. As one of the common treatment methods for ICAS, stent implantation can avoid vascular stenosis leading to hypoperfusion of brain tissue, prevent fibrous cap rupture of unstable plaques, intraplaque hemorrhage, thrombosis, etc., prevent thrombosis from falling off at the stenosis site, reduce the occurrence of distal thromboembolic events, and avoid stenotic plaques directly obstructing perforating vessels [8]. However, SAMMPRIS showed that 14.7% of patients died or had a stroke within 30 days after intracranial artery stenting. In highrisk patients with atherosclerotic intracranial artery stenosis, the early and long-term efficacy of active medical management is higher than that of Wingspan stent implantation. Therefore, the exploration of interventional therapy for intracranial artery stenosis must strictly grasp the indications and contraindications. At present, the vessels that can be treated with stent are limited to the intracranial segment of the internal carotid artery, the M1 segment of the middle cerebral artery (most of which are before the bifurcation, and occasionally reach M2-M3 segment), the intracranial segment of the vertebral artery and the basilar artery, and there are also case reports of the P1 segment of the posterior cerebral artery. During stent treatment, the proximal vessels are less difficult than the distal vessels, and the stenosis of small lumen arteries is more likely to form restenosis or occlusion after stent treatment. Due to the influence of material factors, stents are generally not used for vessels with a diameter <2 mm, and vascular lesions with fewer perforators, non-bifurcation and non-angulation may have better effects. However, there is no good clinical evidence to confirm which vessel will be better treated by stent, which needs our doctors engaged in cerebrovascular intervention to practice and summarize constantly. n addition, after stenting, it is not the end of treatment but the beginning of treatment. Standard antithrombotic therapy after stenting is combined with aspirin and clopidogrel for at least 28 to 90 days, then clopidogrel is discontinued, and aspirin should be taken for life. In the process of strict postoperative drug management and follow-up review, In-Stent Restenosis (ISR) and other complications make it face a new round of challenges.
Conclusion
Angioplasty and stenting of vertebrobasilar artery and large vessel stenosis are technically safe and feasible, and provide alternative treatment options for drug-refractory lesions. Careful patient and device selection in accordance with current AHA/ASA guidelines and the recent SAMMPRIS results may improve clinical outcomes, especially in patients with high rates of disability and mortality in other treatments.
Funding
This work was supported by Natural Science Foundation of Inner Mongolia Autonomous Region [Grants number: 2021MS08108]; Science and Technology Project of Inner Mongolia Autonomous Region [Grants number : 2021GG0114].
References
- Huang HW, Guo MH, Lin RJ, Chen YL, Luo Q, et al. Prevalence and risk factors of middle cerebral artery stenosis in asymptomatic residents in Rongqi County, Guangdong. Cerebrovasc Dis. 2007; 24: 111-5.
- Ingall TJ, Homer D, Baker HL Jr, Kottke BA, O’Fallon WM, et al. Predictors of intracranial carotid artery atherosclerosis. Duration of cigarette smoking and hypertension are more powerful than serum lipid levels. Arch Neurol. 1991; 48: 687-91.
- Wong KS, Ng PW, Tang A, Liu R, Yeung V, et al. Prevalence of asymptomatic intracranial atherosclerosis in high-risk patients. Neurology. 2007; 68: 2035-8.
- Chimowitz MI, Lynn MJ, Howlett-Smith H, Stern BJ, Hertzberg VS, et al. Warfarin-Aspirin Symptomatic Intracranial Disease Trial Investigators. Comparison of warfarin and aspirin for symptomatic intracranial arterial stenosis. N Engl J Med. 2005; 352: 1305-16.
- Chimowitz MI, Lynn MJ, Derdeyn CP, Turan TN, Fiorella D, et al. SAMMPRIS Trial Investigators. Stenting versus aggressive medical therapy for intracranial arterial stenosis. N Engl J Med. 2011; 365: 993-1003.
- Sundt TM Jr, Smith HC, Campbell JK, Vlietstra RE, Cucchiara RF, et al. Transluminal angioplasty for basilar artery stenosis. Mayo Clin Proc. 1980; 55: 673-80.
- Marks MP, Marcellus ML, Do HM, Schraedley-Desmond PK, Steinberg GK, et al. Intracranial angioplasty without stenting for symptomatic atherosclerotic stenosis: Long-term follow-up. AJNR Am J Neuroradiol. 2005; 26: 525-30.
- YU S C H, LAU T W W, WONG S S M, et al. Long-term evolutionary change in the lumen of intracranial atherosclerotic stenosis following angioplasty and stenting [J]. Oper Neurosurg (Hagerstown). 2018; 14: 128-138.