Research Article
Volume 2, Issue 7
The Virtual Medical Care of Heart Failure, An Overview
Jose Ferrer Costa1*; Leomar Colmenares Hernandez2
1General Practitioner, Badalona Serveis Assistencials, Spain.
2Family Medicine residents, Badalona Serveis Assistencials, Spain.
Corresponding Author:
Jose Ferrer Costa
Email: jfcosta@bsa.cat
Received : Jun 09, 2023 Accepted : Jul 21, 2023 Published : Jul 28, 2023 Archived : www.meddiscoveries.org
Citation: Jose FC, Hernandez LC. The Virtual Medical Care of Heart Failure, An Overview. Med Discoveries. 2023; 2(7): 1058.
Copyright: © 2023 Jose FC. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
We’re currently witnessing an exponential surge in technological advancements, especially in the fields of Virtual Reality (VR) and Artificial Intelligence (AI). These technologies have found a dynamic role within the medical and healthcare sector, expanding the boundaries of patient care, diagnosis, treatment, and even medical education.
From enabling surgeons to meticulously plan complex procedures using VR, to AI’s role in patient treatment optimization, these modern tools have opened unprecedented opportunities in managing heart failure. They’ve even extended their impact to supporting patients’ physical and mental wellbeing.
The current digital transformation in healthcare is an opportunity to re-humanize medicine. The role of physicians and nurses is irreplaceable; their compassion and empathy are the beating heart of patient care. The challenge, and the opportunity, lies in learning to harmonize technological support with this indispensable human component. This unique fusion could redefine the future of healthcare, augmenting our abilities while keeping us grounded in our shared humanity.
Keywords: Virtual reality; Augmented reality; Artificial intelligence; Heart failure; Treatment adherence; Virtual medical training; Surgical training; Patient recovery.
Virtual reality
Virtual Reality (VR) is a computer-based simulated experience that can be more or less immersive depending on the hardware used to access it. This virtual environment allows the user to interact with scenarios and objects that simulate reality, thanks to the use of advanced computer technology.
Augmented Reality (AR), on the other hand, is the confluence of VR and the tangible world around us. It overlays digitally generated elements onto our real-world surroundings, enabling interaction with these virtual components. AR engages various sensory modalities, extending beyond the visual to include auditory and tactile experiences [1].
When AR evolves further, allowing for seamless interaction between the real and virtual elements within a shared environment, it becomes Mixed Reality (MR). In this space, 3D virtual content reacts to the user as real-world objects would, enhancing the depth of interaction and immersion [2].
Haptics
Haptics is another technology associated with this virtual or augmented reality. It’s based on tactile feedback using sophisticated devices and software, and can produce a differentiation between materials such as bone and soft tissue, giving a more realistic sense of touch in a simulation [3-5].
Artificial intelligence
The roots of Artificial Intelligence (AI) trace back to the pioneering insights of Alan Turing in 1947, who envisioned a future enlivened by intelligent machines. Turing posited, “What we want is a machine that can learn from experience,” an idea that has, over the decades, sparked a revolution [6].
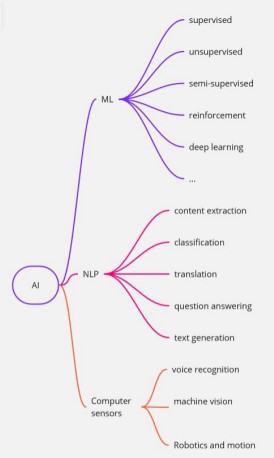
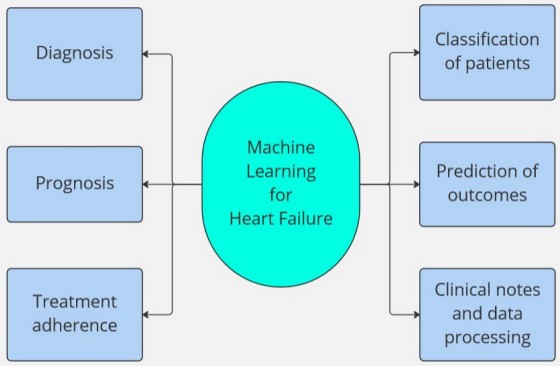
Since Turing’s prescient statement, AI has charted a transformative journey, morphing from the theoretical to the palpable. Today, AI’s prowess lies in its ability to dissect data, decipher patterns, and make data-driven decisions by harnessing advanced mathematical algorithms. The backbone of this intelligent processing lies in two key techniques: Machine Learning (ML), which involves AI systems learning and improving from experience, and Natural Language Processing (NLP), which enables AI to understand and interact using human language. But AI’s power extends beyond these, with a plethora of systems designed to process varied inputs, creating a vast matrix of possibilities (Figure 1).
Machine Learning (ML) algorithms are able to sift through structured data, such as patient registries or medical images. They can tease out patterns, trends, and even make predictions about a patient’s disease progression or potential outcomes, providing valuable insights that might otherwise remain hidden [7].
Natural Language Processing (NLP) is another tool in AI’s arsenal, and it’s particularly adept at making sense of unstructured data, such as clinical notes or medical journals. It can organize this information into structured data, that can be further analyzed by AI systems, revealing meaningful conclusions [8]. This can be especially beneficial when the information is crucial for research purposes.
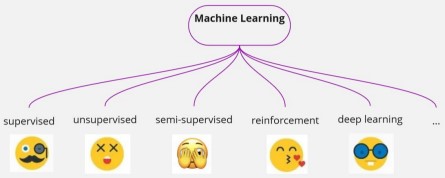
The ways in which machines learn are varied and complex. The three basic categories are supervised, unsupervised, and semi-supervised learning, but many more sub-categories have evolved over the years, such as reinforcement learning and deep learning. For a more in-depth look into these learning methods, refer to comprehensive reviews such as the ‘Machine-LearningBased Disease Diagnosis: A Comprehensive Review’ [9].
Artificial intelligence has an impressive tenure in the field of medicine, predating both VR and AR. Its versatile applications span across the medical spectrum, enhancing areas such as medical training, education, patient diagnosis, and ongoing monitoring [10-12]. The source of the information used by the AI can come from the healthcare system or directed from the patients using electronic devices as medical monitors.
Wearables
When we think about the new digital tools we probably remember someone using a smart watch. These handy gadgets exemplify the potent synergy of hardware and AI. Thanks to intricate AI algorithms, these devices have stepped beyond the realm of consumer electronics and found their niche in health diagnostics, enhancing capabilities and improving clinical decision-making through automated cardiac measurements [13].
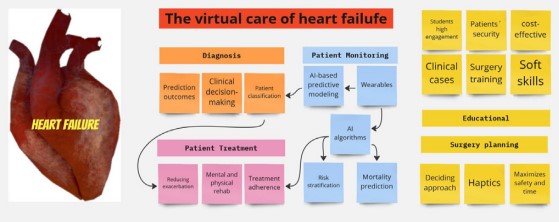
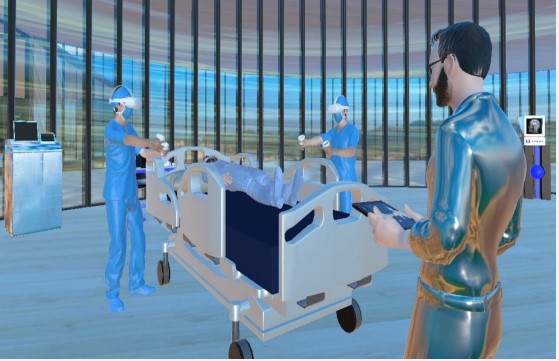
The interplay of VR, AR, MR, AI, and ML creates a comprehensive ecosystem for virtual patient care. Certain tools shine in specific applications: VR and AR excel in medical training, while AI and ML are invaluable in patient care. To distill the breadth of applications, we’ve organized their use into three primary categories: patient care, diagnostics, and education/ training (Figure 3).
Patient care
New technologies with telemonitoring and interventional characteristics can influence habits concerning exercise, nutrition and medication adherence. The association of smart wearables and AI data analyzing can be used to optimize their follow up. These tools can also support their physical and mental health.
The ML algorithms can monitor, process and organize physio-psychological and behavioral data, generating alerts in both directions: For the clinicians it can generate alerts when critical data is detected at home and, for the patients and caregivers, notifications about medication intake with possibility to track the weekly consumption, exercise and nutrition routine, between other uses [14].
When comparing the management of HF patients with Machine learning versus conventional clinical methods, we find 6 main areas where ML can make a positive impact [15] (Figure 4).
Treatment adherence
Poor medication compliance is a common problem with HF patients, leading to increased exacerbations, reduced physical function, higher readmission and mortality rates [16,17]. In a review from 2019 [18] they found that the lower medication adherence is directly related to the patients´ low level of literacy, which leads to higher rehospitalization and death rates.
The use of ML to help with the adherence of medication has been studied for a long time. It can stratify the data and give us evidence-based conclusions to help make clinical decisions [19]. In heart failure one of the biggest utilities of AI is in this line. It gives us organized information to understand each patient’s medication-taking behaviors, consider the side effects and assess health literacy. All this insight can bring us conclusions to reduce the complexity of the treatment and plan a better follow strategy [20].
This use of ML is very connected with the patient’s classification and prediction of outcomes, the origin of the data and the way it is analyzed is very similar. In a recent review about the use of AI in the management of heart failure patients, it has been concluded that it may play an important role in reducing adverse outcomes [21]. Machine learning predictive models can accurately prognosticate different types of clinical progress among this population. The combined approach using ML tools during hospitalization and in outpatient care may result in clinical benefits, reducing readmission after hospitalization [22].
Pain management
Virtual reality is also found to be useful in the work of relieving chronic pain. Immersive VR has been found to effectively distract and thus relieve pain for such patients, especially when the use of anesthesia or sedation is contraindicated. For hospitalized patients with heart failure it can be effective as a nonpharmacologic adjuvant for pain management [23,24].
Therapeutic Applications: Physical and Psychological Dimensions
Virtual reality can be used for physical and cognitive rehabilitation in heart failure patients. It can speed up recovery time by making an exercise routine easier for patients. By constructing alternative realities, VR helps in distracting patients from discomfort and pain during exercise routines, subsequently encouraging their participation and potentially accelerating recovery [25].
An array of studies highlight the potential of cognitive stimulation through VR, showing positive impact in neuropsychological stimulation and rehabilitation programs specifically targeting executive functions. Despite the scarcity of larger populationbased studies, and the need for more rigorous research designs, heart failure patients have demonstrated a good acceptance of these systems, which have proven to be safe and show potential to improve attention [26,27].
Despite the many studies, trials and reviews that show impressive potential in increasing patient care, there is currently considerable heterogeneity. It is important to highlight that we need more organized specific parameters and directives. There should be more structured models and evaluation rigor for studies using AI and ML in any specific pathology [28].
Immersive virtual reality exergames, the fusion of exercise and games, can significantly enhance physical exertion while promoting positive experiences. Advancements in technology promise to minimize side effects such as nausea, dizziness, eye fatigue, and headaches, in the future [29].
Another significant aspect to consider is the mental wellbeing of patients with heart failure, given that the condition’s symptoms can often be restrictive. VR therapies have shown potential in fostering relaxation and wellbeing. Again we have the same limitation when we look further into the literature: A lack of randomized controlled trials and longer-term evidence. More structured guidelines for clinical research are needed to build more robust evidence. Despite that, a positive impact reported on emotional, social, and functional aspects of wellbeing can be seen, especially when the group studied is suffering from chronic pain or other situations that negatively impact their general wellbeing [30-32].
Diagnosis
Heart failure is in its essence a clinical diagnosis. Nevertheless echocardiography is a basic tool in evaluating the cardiac structure and function [33]. ML based systems have been developed to help improve the precision of its interpretation, functioning as an intelligent assistant for the sonographer [34]. The use of AI in echocardiography has the most capabilities in recognizing the standard section, cardiac cavity automatic segmentation, functional left ventricle assessment, and cardiac disease diagnosis [35,36].
AI has matched or even surpassed experienced human counterparts in evaluating echocardiography in some studies [37]. There are still some legal and ethical limitations to its implementation. The human expert should be the one controlling the diagnostic process, getting support from AI systems to guide detection, functional evaluation, and disease diagnosis on request.
In the 2021 guidelines for the diagnosis and treatment of acute and chronic heart failure review of the European Society of Cardiology [38], we can find modern gadgets that can assist health professionals to correctly diagnose and early detect a sign of heart failure. Information collected by different devices (ECG recorders by mobile-health/smartphones, implantable loop recorders, image and genetic tests) can be analyzed by AI and find the origin of the heart failure condition. They can also impact the costs by reducing follow-up visits and re-hospitalizations by an early detection of negative outcomes [39].
Educational/training Surgery training and planning
Using 3D printed models based on real patients’ imagery has been used for decades to allow surgeons to decide the best surgical approach. VR and AR are the natural evolution of that tool, especially for the environmental advantages and extra features that these new technologies can bring.
Some simulations offer the possibility to interact with the virtual objects in a more realistic way, using advanced haptic technology. It can be produced by simple stimuli like a vibration or rumble in a game controller or much more sophisticated elements such as some haptic gloves that can simulate the physical tension of a specific tissue, producing a braking force that blocks the finger’s movement [40].
In the surgical training field, the use of haptics technology is growing fast, since the sense of touch is primordial when a surgeon is performing surgery [41]. While the technology already exists, further improvements are needed for the implementation of these systems as a rule. Not only the costs, but the fine tuning of complex surgical procedures need time to be fully possible in a virtual simulation [42].
The data is compiled from CT, MRI and ultrasound scans, which are complemented by VR and haptics. The reconstruction looks and feels like the actual patient when in surgical surroundings. It’s not a new technology and has been used for planning and training surgical procedures for decades. One of its first applications was building the first augmented reality systems at U.S. Air Force laboratories in 1992 [43].
When planning complex operations, such as neonatal cardiological procedures, VR and AR help the surgical team walk through the whole surgery and rehearse their planned intervention. This maximizes safety and reduces time by minimizing surprises [44].
Learning engagement
Part of the learning process in an educational program depends on its capacity to retain the attention of the students. When you transform 2D objects into 3D interactive ones, and use them in an immersive digital environment, the learning experience is much more engaging [45].
Using immersive VR simulations with headsets has the advantage of fully engaging the user in the simulated environment and giving them a more thorough experience [46]. Another important aspect when planning an educational program is its effectiveness as a competency-based system, which also can be enhanced [47].
VR simulations offer students a safe environment to perform skills and train protocols, some contexts would be expensive and dangerous to simulate in real life. Amongst the many skills we can teach in VR are procedures performance, clinical assessment and decision-making, team work, learning empathy, etc [48].
The technology is advancing fast. Training soft skills such as clinical decision-making or diagnosing is technically easier to do, but we can also find good results in training procedural skills such as a catheter training VR simulation for learning percutaneous coronary interventions, as in this study [49].
Final comments
As we navigate through the technological frontier in healthcare, we’re constantly amazed by the rapid development and utility of these innovative tools. AI and VR are revolutionizing our understanding and treatment of complex diseases such as heart failure, yet they are only tools in our ever-expanding medical kit.
Their acceptance, especially within public healthcare systems, is still a hurdle to overcome. The issues are multifaceted, from the cost of the technology to digital literacy and integration with the traditional clinical workflow. Not to mention the everpressing concern of data privacy in our increasingly connected world.
While we benefit from the scientific knowledge gathered by these intelligent machines, we must remember the essence of healthcare. It’s not just about accurate diagnosis and effective treatment. It’s about the human connection that lies at the heart of all medical care.
In our pursuit of modern medical marvels, we must not forget that we’re humans treating fellow humans. We’re deciphering their stories of suffering, putting together the pieces of their health puzzles, and offering them a hand to hold through their healing journey.
These digital tools, no matter how advanced, should augment rather than replace the intimate patient-doctor relationship. After all, the art of medicine lies not just in the science of disease, but in the compassionate care of the person bearing it.
As we stride forward in this exciting era of medical technology, let’s ensure we keep sight of the human soul amid the digital noise. Because it is our empathy and care that truly heal, something no machine can replicate.
Ethics considerations: Addressing the ethical considerations is crucial for the successful integration of AI and VR in healthcare. It will require collaboration among healthcare professionals, technologists, ethicists, and policymakers to create guidelines and regulations that ensure these technologies are used ethically and responsibly.
Declarations
Some points that can be important considering are:
-The Pandora's Box of Data Privacy: Our brave new world of AI and VR raises enormous questions around the sanctity of personal data. When we immerse ourselves into a VR therapy session or submit our vitals to an AI diagnostic tool, a wealth of private health information is generated, and with it emerges an imperative to protect this sensitive data from unauthorised access. Navigating this maze of privacy is as paramount as the technologies themselves.
- Consent: Patients need to understand and agree to how their health data is being used. We need to be clear with them about who is using their information and why.
- Bias: AI uses data to make decisions. If the data we give it is biased (for example, if it's mostly from a certain group of people), then the AI could make biased decisions too. We need to make sure we use diverse and fair data.
- Transparency: AI can be complicated and hard to understand. We need to find ways to explain how AI makes decisions, especially when it disagrees with human experts.
- Over-reliance on Technology: While AI and VR are useful tools, we can't forget to use our own skills too. We also need to be prepared for when technology breaks or fails.
- Responsibility: If an AI makes a mistake that harms a patient, who is to blame? This is a difficult question that we need to figure out as we use more AI in healthcare.
- Equity: AI and VR are amazing tools, but we need to make sure everyone can use them. They shouldn't be something only rich people or certain groups can benefit from.
References
- Yeung AW, Tosevska A, Klager E, Eibensteiner F, Laxar D, StoyanovJ, Glisic M, Zeiner S, Kulnik ST, Crutzen R, Kimberger O. Virtualand augmented reality applications in medicine: analysis of thescientific literature. Journal of medical internet research. 2021;23: e25499.
- Morimoto T, Kobayashi T, Hirata H, Otani K, Sugimoto M, et al.XR (extended reality: Virtual reality, augmented reality, mixedreality) technology in spine medicine: status quo and quo vadis.Journal of Clinical Medicine. 2022; 11: 470.
- Enayati N, De Momi E, Ferrigno G. Haptics in robot-assisted sur-gery: Challenges and benefits. IEEE reviews in biomedical engi-neering. 2016; 9: 49-65.
- He L, Maiolino P, Leong F, Lalitharatne T, De Lusignan S, MazdakG, et al. Robotic Simulators for Tissue Examination Training withMultimodal Sensory Feedback. IEEE Reviews in Biomedical Engi-neering. 2022.
- Olsson P, Nysjö F, Rodríguez-Lorenzo A, Thor A, Hirsch JM, et al.Haptics-assisted virtual planning of bone, soft tissue, and vesselsin fibula osteocutaneous free flaps. Plastic and ReconstructiveSurgery Global Open. 2015; 3.
- Copeland, B J (ed.), The Essential Turing. 2020.
- de Mattos Paixão GM, Santos BC, de Araujo RM, Horta M. Ma-chine Learning in Medicine: Review and Applicability. Arq BrasCardiol. 2022; 118: 95-102.
- Buchlak QD, Esmaili N, Bennett C, Farrokhi F. Natural languageprocessing applications in the clinical neurosciences: A machinelearning augmented systematic review. Machine Learning in Clin-ical Neuroscience. 2022; 277-89.
- Ahsan MM, Luna SA, Siddique Z. Machine-Learning-Based Dis-ease Diagnosis: A Comprehensive Review. InHealthcare, MDPI.2022; 10: 541.
- Ramesh AN, Kambhampati C, Monson JR, Drew PJ. Artificial intel-ligence in medicine. Ann R Coll Surg Engl. 2004; 86: 334-8.
- Jiang F, Jiang Y, Zhi H, et al. Artificial intelligence in healthcare:Past, present and future. Stroke and Vascular Neurology 2017; 2:e000101.
- Yasmin F, Shah SMI, Naeem A, Shujauddin SM, Jabeen A, et al.Artificial intelligence in the diagnosis and detection of heart failure: the past, present, and future. Rev Cardiovasc Med. 2021; 22:1095-1113.
- Bachtiger P, Plymen CM, Pabari PA, Howard JP, Whinnett ZI, et al.Artificial Intelligence, Data Sensors and Interconnectivity: FutureOpportunities for Heart Failure. Card Fail Rev. 2020; 6: e11.
- Meystre S. The current state of telemonitoring: A comment onthe literature. Telemedicine Journal & e-Health. 2005; 11: 63-9.
- Bazoukis G, Stavrakis S, Zhou J, Bollepalli SC, Tse G, et al. Machine learning versus conventional clinical methods in guiding management of heart failure patients-a systematic review. Heart failure reviews. 2021; 26: 23-34.
- Al-Tamimi MA, Gillani SW, Abd Alhakam ME, Sam KG. FactorsAssociated With Hospital Readmission of Heart Failure Patients.Front Pharmacol. 2021; 12: 732760.
- Sharma A, Mentz RJ, Granger BB, Heitner JF, Cooper LB, et al. Utilizing mobile technologies to improve physical activity and medication adherence in patients with heart failure and diabetes mellitus: Rationale and design of the TARGET-HF-DM Trial. Americanheart journal. 2019; 211: 22-33.
- Oscalices MIL, Okuno MFP, Lopes MCBT, Batista REA, Campan haro CRV. Health literacy and adherence to treatment of patients with heart failure. Rev Esc Enferm USP. English, Portuguese.2019; 53: e03447.
- Son YJ, Kim HG, Kim EH, Choi S, Lee SK. Application of supportvector machine for prediction of medication adherence in heartfailure patients. Healthcare informatics research. 2010; 16: 253-9.
- Cestari VR, Florêncio RS, Garces TS, Souza LC, Pessoa VL, et al.Mapeamento Dos Aplicativos Móveis Para O Cuidado Na Insu-ficiência Cardíaca: Revisão De Escopo. Texto & Contexto-Enfermagem. 2022; 31.
- Błaziak M, Urban S, Wietrzyk W, Jura M, Iwanek G, et al. An Artificial Intelligence Approach to Guiding the Management of HeartFailure Patients Using Predictive Models: A Systematic Review.Biomedicines. 2022; 10: 2188.
- Mortazavi BJ, Downing NS, Bucholz EM, Dharmarajan K, Manhapra A, et al. Analysis of machine learning techniques for heart failure readmissions. Circulation: Cardiovascular Quality and Outcomes. 2016; 9: 629-40.
- Groninger H, Violanti D, Fisher J, Tefera E, Mete M. Virtual Reality for Pain Management in Advanced Heart Failure: A Randomized Controlled Study (S512). Journal of Pain and Symptom Management. 2022; 63: 911.
- Stewart D, Mete M, Groninger H. Virtual reality for pain management in patients with heart failure: Study rationale and design.Contemporary Clinical Trials Communications. 2019; 16: 100470.
- Verheijden Klompstra L, Jaarsma T, Strömberg A. Exergaming in older adults: A scoping review and implementation potential for patients with heart failure. European Journal of Cardiovascular Nursing. 2014; 13: 388-98.
- Robledo-Castro C, Castillo-Ossa LF, Corchado JM. Artificial Cognitive Systems Applied in Executive Function Stimulation and Rehabilitation Programs: A Systematic Review. Arabian journal for science and engineering. 2022; 1-29.
- Jung M, Gradus-Pizlo I, Berman MG, Moser DK, Rogers JL, et al. Feasibility of a novel virtual reality-based cognitive intervention to improve attention in people with heart failure. Journal of Cardiac Failure. 2018; 24: S74-5.
- Jung C, Wolff G, Wernly B, Bruno RR, Franz M, et al. Virtual and augmented reality in cardiovascular care: state-of-the-art and future perspectives. JACC: Cardiovascular Imaging. 2021.
- Xu W, Liang HN, Zhang Z, Baghaei N. Studying the Effect of Display Type and Viewing Perspective on User Experience in Virtual Reality Exergames. Games Health J. 2020; 9: 405-414.
- Appel L, Ali S, Narag T, Mozeson K, Pasat Z, et al. Virtual reality to promote wellbeing in persons with dementia: A scoping review. J Rehabil Assist Technol Eng. 2021; 8: 20556683211053952.
- Riches S, Azevedo L, Bird L, Pisani S, Valmaggia L. Virtual reality relaxation for the general population: A systematic review. Soc Psychiatry Psychiatr Epidemiol. 2021; 56: 1707-1727.
- Austin PD. The Analgesic Effects of Virtual Reality for People with Chronic Pain: A Scoping Review. Pain Med. 2022; 23: 105-121.
- McDonagh TA, Metra M, Adamo M, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021; 42: 3599-3726.
- Medvedofsky D, Mor-Avi V, Amzulescu M, et al. Three-dimensional echocardiographic quantification of the left-heart chambers using an automated adaptive analytics algorithm: Multicentre validation study. Eur Heart J Cardiovasc Imaging. 2018; 19:47-58.
- Zhang Z, Zhu Y, Liu M, Zhang Z, Zhao Y, et al. Artificial Intelligence Enhanced Echocardiography for Systolic Function Assessment. Journal of Clinical Medicine. 2022; 11: 2893.
- Zhou J, Du M, Chang S, Chen Z. Artificial intelligence in echocardiography: detection, functional evaluation, and disease diagnosis. Cardiovasc Ultrasound. 2021; 19: 29.
- Sehly A, Jaltotage B, He A, Maiorana A, Ihdayhid AR, et al. Artificial Intelligence in Echocardiography: The Time is Now. Reviews in Cardiovascular Medicine. 2022; 23: 256.
- McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, et al. 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: Developed by the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) With the special contribution of the Heart Failure Association (HFA) of the ESC. European heart journal. 2021; 42: 3599-726.
- Zeppenfeld K, Tfelt-Hansen J, de Riva M, Winkel BG, Behr ER, et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Developed by the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC) Endorsed by the Association for European Paediatric and Congenital Cardiology (AEPC). European Heart Journal. 2022; ehac262.
- Baik S, Park S, Park J. Haptic Glove Using Tendon-Driven Soft Robotic Mechanism. Frontiers in bioengineering and biotechnology. 2020; 8: 541105.
- Van der Meijden OA, Schijven MP. The value of haptic feedback in conventional and robot-assisted minimal invasive surgery and virtual reality training: a current review. Surgical endoscopy.2009; 23: 1180-90.
- Traub J, Feuerstein M, Bauer M, Schirmbeck EU, Najafi H, et al. Augmented reality for port placement and navigation in robotically assisted minimally invasive cardiovascular surgery. InIntenational Congress Series. Elsevier. 2004; 1268: 735-740.
- Rosenberg, Louis B. “The Use of Virtual Fixtures as Perceptual Overlays to Enhance Operator Performance in Remote Environments”. 1992.
- Ong CS, Krishnan A, Huang CY, Spevak P, Vricella L, et al. Role of virtual reality in congenital heart disease. Congenital heart disease. 2018; 13: 357-61.
- Herbert VM, Perry RJ, LeBlanc CA, Haase KN, Corey RR, et al. Developing a smartphone app with augmented reality to support virtual learning of nursing students on heart failure. Clinical Simulation in Nursing. 2021; 54: 77-85.
- Barteit S, Lanfermann L, Bärnighausen T, Neuhann F, Beiersmann C. Augmented, mixed, and virtual reality-based head-mounted devices for medical education: Systematic review. JMIR seriougames. 2021; 9: e29080.
- Hamad A, Jia B. How Virtual Reality Technology Has Changed OurLives: An Overview of the Current and Potential Applications and Limitations. International Journal of Environmental Research and Public Health. 2022; 19: 11278.
- Zackoff MW, Young D, Sahay RD, Fei L, Real FJ, et al. Establishing objective measures of clinical competence in undergraduate medical education through immersive virtual reality. Academic pediatrics. 2021; 21: 575-9.
- Voelker W, Petri N, Tönissen C, Störk S, Birkemeyer R, et al. Does Simulation-Based Training Improve Procedural Skills of Beginners in Interventional Cardiology?-A Stratified Randomized Study.
- Zeppenfeld K, Tfelt-Hansen J, de Riva M, Winkel BG, Behr ER, et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Developed by the task force for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death of the European Society of Cardiology (ESC) Endorsed by the Association for European Paediatric and Congenital Cardiology (AEPC). European Heart Journal. 2022; ehac262