Research Article
Volume 2, Issue 6
Epidemiological, Clinical, Echographic and Bacteriological Aspects of Tuberculous Pericarditis in the Mohammed VI University Hospital of Marrakech
Rocyr Junior Ibara-Onguema*; Salma Nafidi; Tibou Camara; Sanae Nehame; Mohammed El Jamili; Saloua El Karimi; Mustapha El Hattaoui
Department of Cardiology and Vascular Disease, Mohammed VI University Hospital, Marrakesh, Morocco.
Corresponding Author :
Rocyr Junior Ibara-On
Email: doc.juneagle@yahoo.fr
Received : Jun 01, 2023 Accepted : Jun 23, 2023 Published : Jun 30, 2023 Archived : www.meddiscoveries.org
Citation: Ibara-Onguema RJ, Nafidi S, Camara T, Nehame S, El Jamili E, et al. Epidemiological Aspects, Clinical, Echographic and Bacteriological Aspects of Tuberculous Pericarditis in the Mohammed VI University Hospital of Marrakech. Med Discoveries. 2023; 2(6): 1050.
Copyright: © 2023 Ibara-Onguema RJ. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Introduction: Tuberculosis is a major public health problem and one of the leading causes of pericarditis. Its prevalence is still high in developing countries. This is a serious condition that can be complicated by tamponade and pericardial constriction. The objective of our study was to describe the epidemiological, clinical and evolutionary characteristics of tuberculous pericarditis cases.
Methods: We conducted a retrospective, descriptive, cross-sectional study of tuberculous pericarditis over a 5-year period from January 2018 to January 2023 in the Department of Cardiology and Vascular Diseases at the Mohammed VI University Hospital in Marrakech. Cases were collected from complete patient records. The variables studied were sociodemographic, clinical and paraclinical.
Results: Among 4250 hospitalizations in the cardiology department, 72 patients presented with pericarditis, i.e. 1.69%. Tuberculous pericarditis accounted for 30.5% of all pericarditis. The mean age was 46.7 ± 16.6 years with extremes ranging from 16 to 77 years. The sex ratio was 1.4 in favor of men. Fluidic pericarditis accounted for 77.3% (17 patients) versus 22.7% (5 patients) for Chronic Constrictive Pericarditis (CCP). The mean time to consultation was 45.7 ± 36.7 days with extremes of 7 to 180 days. A notion of pulmonary tuberculosis was present in 4 patients (18.1%), just like the notion of tuberculosis contagion. Dyspnea, chest pain, and altered general condition were the most frequent complaints. Heart failure was present in 9 patients (52.9%) with fluid pericarditis and in 100% of patients with CCP. Cardiomegaly was present in 16 patients (72.7%) of the total population and decanter appearance in 6 patients (27.2%). QRS microvoltage, negative T waves, and PQ undershift were the most common electrical abnormalities found. The effusions were large in 15 patients (83.4%), the pericardium was thickened and calcified in 6 patients (27.3 %). Tamponade was the mode of presentation in 13 patients (76.4%), the pericardiocentesis score was high with a mean of 9.15 ± 2.5 points. Pericardial puncture-drainage was performed in 16 out of 17 patients (94.1%). All patients had negative HIV serology. Pericardial fluid analysis was performed in 13 patients (76.4%); the fluid was hematic in 7 patients (53.8%) and citrine yellow in 6 patients (46.2%); it was exudative in all our patients and lymphocytic in 6 patients (85.7%). Sputum testing for BAARs was performed in 11 patients of whom 7 were negative (63.6%) and 4 (36.4%) were positive. Gene Xpert of the fluid from 11 patients was positive in 5 patients (45.4%) and patients were started on anti-tuberculosis therapy. Right ventricular collapse, inferior vein dilatation, and microvoltage were significantly associated with an effusion greater than 25 mm.
Conclusion: Tuberculous pericardial disease is frequent and constitutes a serious pathology due to its complications. They affect mostly young subjects, a particular interest should be given to the detection and early treatment of patients.
Keywords: Pericarditis; Tuberculosis; Effusion; Tamponade.
Introduction
Tuberculosis is a major public health problem, according to the WHO 10 million people contracted tuberculosis in 2018, it is responsible for 1.2 million deaths in HIV-negative patients, it is the leading cause of death by a single infectious agent ahead of HIV [1]. Its pulmonary localization remains by far the most frequent; however, extra-pulmonary involvement, particularly in the pericardium, is possible [2]. This is a serious condition that can be complicated by tamponade and pericardial constriction [3]. The objective of our study was to describe the epidemiological, clinical, echographic and evolutionary characteristics of tuberculous pericarditis cases in the cardiology department of the Mohammed VI University Hospital of Marrakech.
Patients and methods
We conducted a retrospective descriptive study with crosssectional data collection from patient files and registers in the Cardiology and Vascular Diseases Department of the Mohammed VI University Hospital of Marrakech over a period from January 2018 to January 2023, i.e. 5 years. The parameters studied were sociodemographic, i.e., age, sex; clinical, i.e., clinical examination data, electrocardiogram, chest radiograph, and cardiac ultrasound. All patients were tested for Acid-Fast Bacilli (AFB) in sputum. The diagnosis of tuberculous pericarditis was retained in all patients presenting signs of tuberculous impregnation, signs of right or global cardiac insufficiency, radiological and echocardiographic signs, associated with indirect biological stigmas of tuberculosis. Anatomopathological examination, when performed, confirmed the diagnosis. Quantitative variables were represented as mean, standard deviation, and extremes; qualitative variables were represented as percentages and numbers using Microsoft Office Excel 2007. Fischer’s exact test and Mann Whitney test were used to compare quantitative and qualitative variables, respectively, with a threshold of positivity of 0.05. A bivariate analysis was performed to compare the different parameters with the size of the pericardial effusion, taking 25 mm as the cutoff.Anonymity and confidentiality were taken into account in the development of this work.
Results
Hospital frequency
Of 4250 patients hospitalized in the cardiology department during the study period, 72 patients or 1.69% of hospitalizations had pericarditis. Among the pericarditis, 22 (30.5%) were of tuberculous origin.
Socio-demographic characteristics
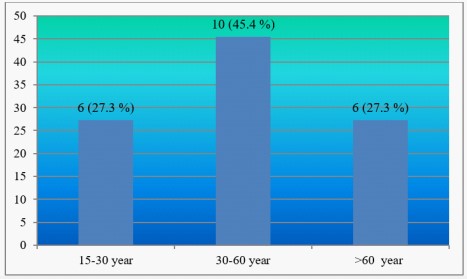
The mean age of our study population was 46.7 ± 16.6 years with extremes from 17 to 77 years. The distribution of patients according to age groups is given in Figure 1.
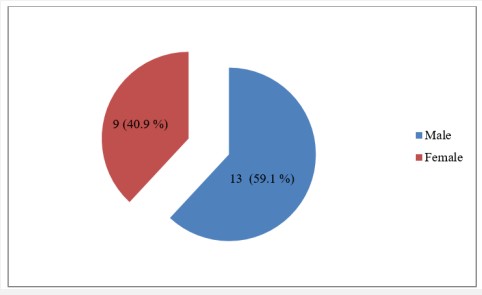
In our series, the sex ratio was 1.4 in favor of men. Figure 2 shows the distribution of patients by gender.
Clinical and paraclinical characteristics
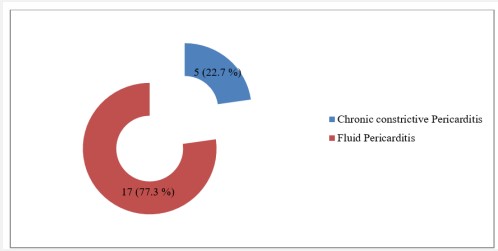
Figure 3 illustrates the distribution of patients according to the evolutive form of tuberculosis. In our series, liquid pericarditis was the dominant form, found in 77.3%.
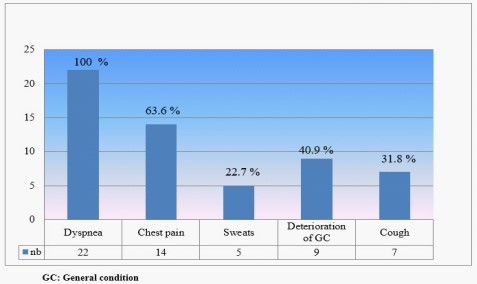
The mean time to consultation since the onset of signs was 45.7 ± 36.7 days with extremes of 7 and 180 days. A history of pulmonary tuberculosis was found in 4 patients (18.1%), 3 of whom had CCP. Concerning the reason for consultation, in our series, dyspnea was present in all our patients, followed by chest pain and alteration of the general state. Signs of right heart failure were found in 9 patients (52.9%) with fluid pericarditis, whereas they were present in all patients with CCP. The distribution of patients according to the reason for consultation is given in figure 4.
Regarding the radiographic appearance, cardiomegaly was present in 16 patients (72.7%), the characteristic decanter heart appearance in 7 patients (41.1%) of fluid pericarditis.
In our study all patients had performed an electrocardiogram. 20 patients (90.9%) were in sinus rhythm and 2 patients were in rapid atrial fibrillation on admission. 14 patients (63.6%) were tachycardic. The distribution of patients according to electrical anomalies is given in Table 1.
Table 1: Distribution of patients according to the type of electrical anomalies.
| ECG parameters | Number | % | |
|---|---|---|---|
| Microvoltage | Yes | 18 | 81,8 |
| No | 4 | 18,2 | |
| Repolarization disorders | ST elevation | 3 | 13,6 |
| Flattened T-waves | 10 | 45,4 | |
| Negative T-waves | 5 | 22,8 | |
| Absence of disorders | 4 | 18,2 | |
| PQ segment sub-offset | Yes | 2 | 9,1 |
| No | 20 | 90,9 | |
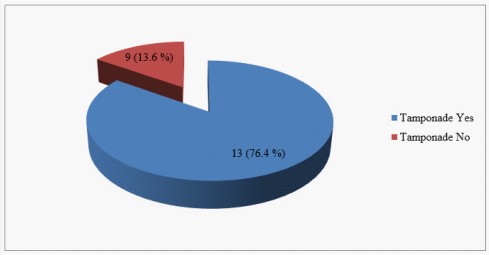
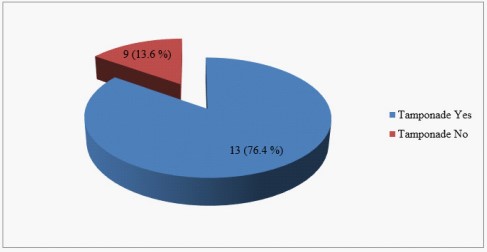
Table 2 shows the distribution of patients according to transthoracic ultrasound data. Of the 17 patients with fluid pericarditis, tamponade was present in 13 patients (76.4%). Figure 5 illustrates the distribution of patients by revealing mode of presentation.
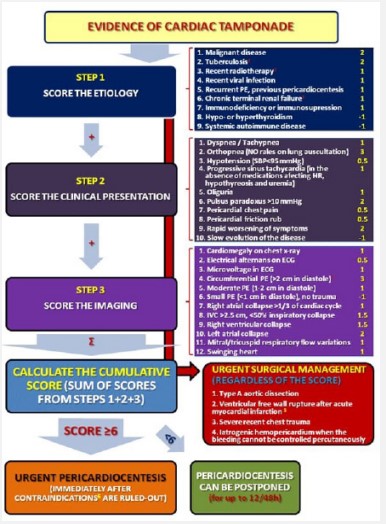
The mean pericardiocentesis score was 9.15±2.5 for all fluid pericarditis. And 16 patients (94.1 %) had pericardial puncture. Figure 6 shows the percentage of patients with an indication for pericardiocentesis.
Pericardial fluid analysis was performed in 13 patients (76.4%).
Table 2: Distribution of patients according to ultrasound data.
| Echocardiographic parameters | Number | % | |
|---|---|---|---|
| Pericardial effusion | Yes | 18 | 81,8 |
| No | 4 | 18,2 | |
| Abundance | Large | 15 | 83,4 |
| Average | 2 | 11,1 | |
| minimal | 1 | 5,5 | |
| Aspect of the pericardium | Thickened/calcified | 6 | 27,3 |
| normal | 16 | 72,7 | |
| Respiratory variations | Yes | 15 | 88,2 |
| No | 2 | 11,8 | |
| Pulmonary hypertension | Yes | 2 | 9,1 |
| No | 20 | 90,9 | |
| IVC dilatation | Yes | 15 | 68,2 |
| No | 7 | 31,8 | |
| Collapse of the RV | Yes | 9 | 40,9 |
| No | 13 | 59,1 | |
| Notch of the OD | Yes | 10 | 45,4 |
| No | 12 | 54,6 | |
IVC : Inferior Vena Cava.
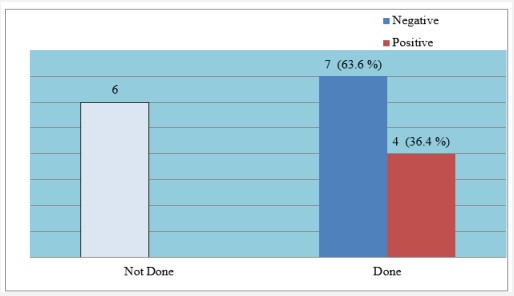
Table 3 shows the distribution of patients by fluid analysis. GeneXpert of pericardial fluid was performed in 11 patients of whom 5 (45.4%) were positive. Sputum analysis for BAARs was performed in 11 of 17 patients (64.7%). BK was detected in 4 patients (36.4%). Figure 7 shows the distribution of patients according to sputum analysis result.
Table 3: Distribution of patients by pericardial fluid analysis.
| Liquid analysis | Number | % | |
|---|---|---|---|
| Pericardial fluid appearance | Hematic | 7 | 53,8 |
| Citrine yellow | 6 | 46,2 | |
| Biochemistry | Exudative | ||
| Transudative | |||
| Cytology (Predominance) |
Lymphocytic | 6 | 85,7 |
| Neurophiles | 1 | 14,3 | |
Table 4 gives the distribution of patients according to the importance of the pericardial effusion to determine in bivariate analysis the factors associated with the size of the effusion. Right ventricular collapse, inferior vein dilatation, and microvoltage were significantly associated with an effusion greater than 25 mm.
Table 4: Factors associated with the importance of the effusion.
| Parameters | Effusion ≥ 25 mm |
Effusion < 25 mm |
P value | |
|---|---|---|---|---|
| Average age | Average | 49,4 | 46 | 0,8 |
| Gender | Male | 5 | 5 | 0,3 |
| Feamle | 6 | 1 | ||
| Respiratory variations | significant | 10 | 4 | 0,5 |
| Not significant | 1 | 2 | ||
| Notch of the right atrium | Present | 7 | 1 | 0,1 |
| Absent | 4 | 5 | ||
| Collapse right ventricule | Yes | 8 | 1 | 0,04 |
| No | 3 | 5 | ||
| Inferior venous cave | Dilated | 11 | 1 | <0,001 |
| Non-expanded | 0 | 5 | ||
| Micro voltage | Yes | 11 | 3 | 0,02 |
| No | 0 | 3 | ||
| T-waves | Flattened | 6 | 1 | 0,1 |
| Negative | 2 | 0 | ||
| Normal | 3 | 5 | ||
Discussion
Tuberculosis is a major health problem in the world in general and in Africa in particular [1]. Although pericardial localization is not the most frequent, it is a serious pathology due to its potentially fatal complications [2-4]. Its prevalence in the general literature is of the order of 1 to 8%, and is more important in HIV-infected subjects [2-6]. In developing countries, tuberculosis is the leading cause of pericarditis [5]. Tuberculous pericarditis mainly affects young subjects under 40 years of age (about 50% in our series); this is in accordance with the data in the literature [1-5]. We found a clear male predominance in our series; in fact, according to the WHO [1], tuberculosis affects both sexes in every age group combined with a male burden above 15 years.However, our data differ from those of some authors [7,8] who report a female predominance in pericarditis of various origins.
The reasons for consultation found in our series corroborate those of the literature [5,7,8]. The electrical changes found in our series are not specific to tuberculosis and are encountered in all cases of pericarditis, as is cardiomegaly, which is indicative of a medium to large pericardial effusion [4-8]. The average delay of consultation is 45 days, this delay of management can be a pejorative element for our patients especially when we know that tuberculous pericarditis evolves rapidly towards chronicity [5]. This shows that there is still much to be done in terms of patient education and awareness.
Fluid pericarditis was found in 77.3% of cases in our series, with a medium to large circumferential effusion in more than half of the cases, which is in line with several authors [4-6]. Tamponade, which is the most dominant revealing form in our series, has also been reported in the literature, especially in developing countries [4-6]. Chest X-ray, electrocardiogram and cardiac ultrasound represent the first diagnostic step [2,3,5,6]. Transthoracic echocardiography remains essential for the positive diagnosis of the effusion and is useful to look for a hemodynamically significant effusion, tuberculous pericarditis can be revealed by an inaugural tamponade (82% in our series) [2,3,5]. The appearance of the fluid found in our series corroborates those of Dybowska et al who found essentially a citrine or hematic, exudative and lymphocytic fluid [5,9]. Right ventricular collapse, inferior vein dilatation, and microvoltage were frequently significantly associated with an effusion greater than 25 mm our series.
However, the etiological diagnosis is often problematic. The diagnosis of tuberculosis is based primarily on epidemiological, clinical and pathological evidence. In our series, para-clinical examinations, notably the search for BK in sputum, was positive when performed in 36.4% of patients. GeneXpert of pericardial fluid was performed in 11 patients of whom 5 (45.4%) were positive. Adenosine deaminase testing is recommended but not always available. Genexpert was performed in 11 patients, i.e. half of our sample, and was positive in 45.4% of cases. It is a crucial examination in the diagnosis of tuberculosis and multidrug-resistant forms. It is described that this examination has moderate sensitivity and high specificity [4,5,10,11]. Other diagnostic means based on the immunological approach to confirm tuberculosis origin are being developed [6,12].
Progression on treatment is a valuable argument in the management of tuberculosis [2,3]. The pericardiocentesis score (Figure 8) was high in 5 patients in our series indicating emergency puncture. On the other hand, it seems that the effusions of tuberculous pericarditis should be drained because of their abundance and rapid reconstitution with risk of pericardial constriction [2-5]. Corticosteroid therapy is routinely recommended for all tuberculous pericarditis to avoid recurrence and progression to CCP [2,3,5]. However, a meta-analysis by George et al [13] demonstrated that the use of corticosteroid therapy did not reduce mortality in tuberculous pericarditis.
The prognosis depends on the speed of diagnosis. Indeed, chronic constrictive pericarditis must always be feared, which in our series was present in 22% of cases.
Conclusion
Tuberculous pericardial disease is frequent and constitutes a serious pathology because of its complications. It affects mostly young patients, a particular interest should be given to the detection and early treatment of patients. Echocardiography plays an important role in management. Pericardial drainage should be routine to avoid progression to chronic constrictive pericarditis. Medical treatment is based on anti-tuberculosis drugs and adjuvant corticosteroid therapy has an important place.
Abbreviations: BK: Bacillus Koch; CCP: Chronic constrictive pericarditis; HIV: Human immunodeficiency virus; WHO: World health organization.
Declarations
Conflict of interest declaration: The authors declare that they have no conflict of interest.
Ethical statement: Our study is retrospective, so an ethical opinion is not required. Anonymity and confidentiality were respected.
Funding statement: The authors declare that they have not used any funding for this work
References
- World Health Organization (WHO). Global TB Report 2019.
- Y Adle, P Charron, M Imazio, L Badano, G Baron-Esquivias, et al. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases. European Heart Journal. 2015; 36: 2921-2964.
- B Karpuz, V Duchatelle, M Tapponnier, R Alexe, C Sierro et al. Pericardial diseases: What’s new in 2016? Rev Med Suisse. 2016; 12: 1475-1478.
- SA Chang. Tuberculous and Infectious Pericarditis. Cardiol Clin. 2017; 35: 615-622.
- JP Lopez-Lopez, EL Posada-Martínez, C Saldarriaga, F Wyss, CI Ponte-Negretti, et al. Tuberculous and the heart. J Am Heart Assoc. 2021; 10: e019435.
- Kishendree Naicker, Mpiko Ntsekhe. Tuberculous pericardial disease: a focused update on diagnosis, therapy and prevention of complications. Cardiovasc Diagn Ther. 2020; 10: 289-295.
- B Dembélé, M Diakité, B Diarra, N Sidibé, A Sangaré et al. Panorama of Pericarditis at the Reference Health Center of Commune I of the District of Bamako. Health Sci. Dis. 2022; 23: 34-36.
- UD Kombila, EE Nzengue, A Kinga, JR Mackanga, D Mounguengui et al. Place of tuberculosis in acute pericarditis in Gabonese hospitals. Rev Pneumol Trop. 2017; 27: 3-8.
- M Dybowska, K Błasinska, J Gatarek, M Klatt, E AugustynowiczKopec, et al. Tuberculous Pericarditis: Own Experiences and Recent Recommendations. Diagnostics. 2022; 12: 619.
- Yu G, Ye B, Chen D, Zhong F, Chen G, et al. Comparison between the diagnostic validities of Xpert MTB/RIF and interferon-γ release assays for tuberculous pericarditis using pericardial tissue. PLoS ONE. 2017; 12: e0188704.
- G Yu, F Zhong, Y Shen, H Zheng. Diagnostic accuracy of the Xpert MTB/RIF assay for tuberculous pericarditis: A systematic review and meta-analysis. Plos ONE. 2021; 16: e0257220.
- G Isiguzo, E Du Bruyn, P Howlett, M Ntsekhe. Diagnosis and Management of Tuberculous Pericarditis: What Is New ? Current Cardiology Reports. 2020; 22: 2.
- IA George, B Thomas, JS Sadhu. Systematic review and metaanalysis of adjunctive corticosteroids in the treatment of tuberculous pericarditis. Int J Tuberc Lung Dis. 22: 551-556.