Research article
Volume 2, Issue 6
Rate of Same-Day Antiretroviral Therapy Initiation and its Predictors among Newly-Diagnosed HIV-Positive Patients in a District Hospital in Douala, Cameroon
Derrick T Efie1,2; Nsagha Dickson1; Denis Zofou1; Calson Ambomatei2*; Fatimatou M Efie3
1Department of Public Health and Hygiene, Faculty of Health Sciences, University of Buea, Cameroon.
2Department of Health search Association, Cameroon.
3Department of Bonaberi Baptist Hospital, Cameroon Baptist Convention Health Board, Douala, Cameroon.
Corresponding Author:
Calson Ambomatei
Email: calsonambomatei@yahoo.com
Received : May 05, 2023 Accepted : Jun 01, 2023 Published : Jun 10, 2023 Archived : www.meddiscoveries.org
Citation: Efie DT, Dickson N, Zofou D, Ambomatei C, Efie FM. Rate of Same-Day Antiretroviral Therapy initiation and its Predictors among Newly-Diagnosed HIV-Positive Patients in a District Hospital in Douala, Cameroon. Med Discoveries. 2023; 2(6): 1043.
Copyright: © 2023 Ambomatei C. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Aim: The fight against HIV/AIDS remains a global health priority. In 2015, in a bid to control the pandemic, the World Health Organization adopted the “Treatment for All” strategy aimed at guaranteeing the placement of all persons living with HIV (PLWHIV) on Antiretroviral Therapy (ART). ART, especially when started early following diagnosis, decreases the number of AIDS-related deaths and allows PLWHIV to lead healthy lives. This paper aims to determine the rate of same-day ART initiation, assess the factors that favor same-day initiation, and identify the reasons for delayed initiation among people newly diagnosed with HIV in a District Hospital in Douala, Cameroon.
Materials and methods: We conducted a retrospective case note review of 526 files of people diagnosed with HIV between January 2020 and December 2021 at Cite des Palmiers District Hospital in Douala, Cameroon, and interviewed 464 of them. Data on demographic char-demographic characteristics, year of HIV diagnosis, date of ART initiation, and reasons for missed initiations were analyzed using SPSS version 25 and the threshold for statistical significance was set at P≤0.05.
Results: A total of 526 people were diagnosed with HIV at this District Hospital during the study period, of which 350 (66.5%) [95% CI: 62.3, 70.5] were females. The mean age was 36.33 ± 12.52 years and the mean BMI was 23.93 ± 4.43 kg/m2. A total of 404 patients were started on ART on the same day of HIV diagnosis, giving a same-day ART initiation rate of 76.8% [95% CI: 73.0, 80.3]. The median time to ART initiation for patients who did not start ART on the same day was 6 days (IQR: 12 days). Thirty-two (6.1%) patients had not started ART at the end of the study period. The female sex, the 10-19 years age group, pregnancy or breast-feeding, and living within the same health district as the healthcare facility were independently associated with same-day ART initiation. The reasons for delayed ART initiation were either patient dependent (refusal, need to discuss with partner before initiation, and fear of side effects of drugs), healthcare provider-dependent (referral and nondisclosure of results), and hospital management-dependent (inability to ensure the constant availability of drugs).
Conclusion: The rate of same-day antiretroviral therapy initiation at the Cite des Palmiers District Hospital was 76.8%. More than 85% of patients diagnosed with HIV were put on treatment within 14 days of diagnosis, with patients’ poor health condition being the main factor associated with delayed initiation.
Introduction
In the past, antiretroviral therapy (ART) for the human immunodeficiency virus (HIV) infection was delayed until a patient's CD4 count fell below a certain value (such as 200 cells/mm3), which led to a high rate of opportunistic infections [1]. Prior to 2013 in Cameroon, eligibility for ART was based on the patient’s CD4 count at diagnosis. In 2015, the World Health Organization (WHO) recommended the “HIV Treatment for All” strategy as a global approach to control the HIV/AIDS pandemic and in 2016, the Cameroon national guidelines evolved to adopt the HIV Treatment for All policy called “test and treat” locally [2]. Placing people living with HIV (PLWHIV) on ART decreases the number of AIDS-related deaths and allows these people to lead healthy lives. Antiretroviral drugs (ARV) drugs were made available free of charge to those who needed them in Cameroon since 2007, and as of 2020, the country had more than 150 clinics that provided ART [3].
The timing of ART initiation and its impact on clinical and microbiologic outcomes has been controversial in evaluations of the benefit of therapy and of the associated short-term and long-term complications and costs. The WHO recommends the rapid initiation (within 7 days of HIV diagnosis) of ART for people newly diagnosed with HIV, with the option to start treatment on the day of diagnosis (same-day ART) after eliminating clinical reasons to delay treatment [4]. Same-day ART initiation and rapid ART initiation has been presented as a key strategy for attaining the 2030 targets of the Joint United Nations Programme on HIV/AIDS (95-95-95 targets) [5].
The benefits of starting ART on the same day of HIV diagnosis include improvements in treatment uptake and HIV care retention, faster viral suppression, halting further sexual transmission of HIV, and better clinical outcomes [6-8]. In countries with the universal provision of ART such as Cameroon, the early initiation of ART reflects, at least to some extent, the success of HIV care and treatment. Late ART initiation reduces the chances of achieving viral suppression, favors the continuous clinical progression of HIV, increases AIDS and non-AIDS-related morbidity and mortality, and heightens the chances for treatment-related adverse events [9-12]. Little is known about the effectiveness of the “test and treat” strategy as well as the factors that can favor or hinder this approach in Cameroon.
Thus, in this study, we determined the rate of same-day ART initiation, assessed the factors that favor same-day ART initiation, and identified the reasons for delayed initiation among people newly diagnosed with HIV in an urban district hospital in Cameroon.
Materials and methods
Study design, setting, and population
We conducted a mixed study involving a retrospective case note review of 526 files of people newly diagnosed with HIV between January 2020 and December 2021 at the Cite des Palmiers District Hospital in Douala, Cameroon, and a questionnaire-based interview of 464 of PLWHIV. The Cite des Palmiers District Hospital is a 3rd category public hospital with 10 units located within the Cite des Palmier Health District, one of the 24 health districts in the Littoral Region of Cameroon [13].
Study procedures and data collection
All patients’ records within the study period were studied consecutively. Patients who were not initiated on the same day of HIV diagnosis and who were still in care were identified and invited to participate in a questionnaire-based interview during their next appointment. During this cross-sectional phase of the study, an exhaustive approach was used and all patients aged above 21 years who were diagnosed with the HIV infection between January 2020 and December 2021 and who were still in care during the study period were approached. From the HIV treatment registers, the next appointment dates for HIV-positive patients between January 2020 and December 2021 were identified and recorded. An agenda was established in which patients were classified according to their appointment days. On each appointment day, the group of eligible patients who showed up for ARV pick-up were approached through a nonprobability convenient and exhaustive sampling method and invited to take part in a questionnaire-based interview using a pretested questionnaire. A total of 464 respondents were included in this phase.
A Structured pretested data extraction form was used to extract the desired data during the records review. The form was divided into three sections to ease the data extraction process. The first section focused on the demographic characteristics of patients including sex, age, marital status, highest level of education, employment status, and year of diagnosis. The second section summarized information on the clinical characteristics of patients such as the WHO clinical stage at diagnosis, weight and height at diagnosis, the presence of opportunistic infections at diagnosis (including TB, meningitis, and severe anemia). In the third section, we recorded data on the delay in initiation (date of HIV diagnosis and date of ART initiation), and the documented reasons for not initiating the clients on that day (for those with missed same-day initiation). Ethical approval was obtained from the Institutional Review Board of the Faculty of Health Sciences of the University of Buea. Administrative authorizations were obtained from the Regional Delegation of Public Health for the Littoral, the Cite des Palmiers Health District, and the Cite des Palmiers District Hospital, and verbal consent was obtained from all the participants prior to their inclusion.
Statistical analysis
The collected data were entered into an Epi Info7 database and exported to SPSS version 25 for analysis. Multiple imputation by chained equations was used to deal with missing values [14]. All continuous variables were reviewed for normality using the Shapiro-Wilk test based on a probability threshold of p≥0.1. Categorical variables are summarized as frequencies and percentages (with frequency tables and charts) while continuous variables are presented as means and standard deviations. Pearson’s χ2 test was used to determine differences between categorical variables while Student’s t-test was used to determine differences between continuous variables.
We included all variables measured before treatment initiation in the bivariate analysis and used Chi squared tests to determine the association between the different independent variables and the response (same-day initiation). All variables that were associated with the response with a probability threshold of p<0.2 were considered significant and included in the multivariate analysis. At the end of the bivariate analysis, the following variables were retained for the multivariate analysis: sex, pregnancy and breastfeeding status, highest educational level, age group, employment status, and marital status.
During the multivariate analysis, a binary logistic regression model was used to assess the predictors of same-day ART initiation compared to delayed ART initiation. Before running the model, model fitting was ensured by verifying the -2 Log Likelihood criteria in a reduced model. This reduced model was confirmed to be valid and equivalent to the final model since the omission of an effect from the final model did not increase the degrees of freedom in the reduced model. During the regression analysis, the dependent variable, which was a dichotomous variable, was the timing of ART initiation. The two possibilities were either initiated on the same day or not initiated on the same day. The reference category was patients not initiated on the same day, and those in this category were compared with patients initiated on the same day subcategorized on a nominal scale within the different variable categories. We controlled for confounders by including all the variables in the model and only removing variables if the corresponding change in the odds ratio was less than 10%.
Results
General characteristics of participants
Of the 526 patient records we consulted, 176 (33.5%) [95% CI: 29.5, 37.7] belonged to male patients. The mean age of the participants was 36.3 ± 12.5 years and the mean BMI was 23.9 ± 4.43 kg/m2. Twenty-seven (5.2%) [95% CI: 3.4, 7.4] participants were less than 20 years old while 69 (13.1%) [95% CI: 10.4, 16.3] were above 50 years of age. Participants’ general characteristics are shown in Table 1.
Table 1: General characteristics of participants.
| Variables | Categories | Frequency n (%) (N = 526) | 95% Confidence I. |
|---|---|---|---|
| Sex | Male | 176 (33.5) | 29.5 – 37.7 |
| Female | 350 (66.5) | 62.3 – 70.5 | |
| Marital status | Concubine | 48 (9.3) | 6.9 – 12.1 |
| Divorced | 9 (1.7) | 0.8 – 3.3 | |
| Married | 125 (24.2) | 20.5 – 28.1 | |
| Single | 296 (57.3) | 52.9 – 61.6 | |
| Widow | 39 (7.5) | 5.4 – 10.2 | |
| Highest level of education | No Formal Education | 26 (5.8) | 3.8 – 8.3 |
| Primary | 73 (16.2) | 12.9 – 19.9 | |
| Secondary | 262 (58.0) | 53.3 – 62.6 | |
| University | 91 (20.0) | 16.5 – 24.1 | |
| Employment status | Employed | 116 (23.1) | 18.6 – 25.8 |
| Retired | 4 (0.8) | 0.2 – 1.9 | |
| Unemployed | 382 (76.1) | 68.6 – 76.4 | |
| Disclosure of status to partner | Not disclosed | 256 (66.0) | 61.0 – 70.7 |
| Disclosed | 132 (34.0) | 29.3 – 39.0 | |
| Residence | Outside the Health District | 194 (36.9) | 32.7 – 41.2 |
| Within the Health District | 332 (63.1) | 58.8 – 67.3 | |
| Age group (years) Mean: 36.3 SD: 12.5 |
<10 | 13 (2.5) | 1.3 – 4.2 |
| 10 – 19 | 14 (2.7) | 1.5 – 4.4 | |
| 20 – 29 | 138 (26.3) | 22.6 – 30.3 | |
| 30 – 39 | 193 (36.8) | 32.6 – 41.0 | |
| 40 – 49 | 98 (18.7) | 15.4 – 22.3 | |
| ≥50 | 69 (13.1) | 10.4 – 16.3 | |
| BMI Group Mean: 23.9 D: 4.43 |
<18.5 | 32 (7.3) | 4.3 – 8.7 |
| 18.5 – 24.9 | 250 (57.2) | 44.6 – 63.5 | |
| ≥ 25.0 | 155 (35.5) | 26.4 – 39.6 |
Clinical profiles of participants
Forty-five (8.6%) [95% CI: 6.3, 11.3] of the patients were either pregnant or breastfeeding at the time of diagnosis and were diagnosed in the context of the prevention of mother-to-child transmission of HIV (PMTCT). Of the 526 patients, 350 (69.4%) [95% CI: 65.2, 73.4] were diagnosed with WHO clinical stage I HIV while 88 (17.5%) [95% CI: 14.2, 21.1] presented with advanced stages of the disease (WHO clinical stage III & IV) at diagnosis. The clinical profiles of our study participants are shown in Table 2.
Effectiveness of the “test and treat” strategy
Of the 526 people newly diagnosed with HIV over the two-year study period, 404 were initiated on ART on the same day they were diagnosed, giving an ART same-day initiation rate of 76.8% [95% CI: 73.0, 80.3], 468 (89%) [95% CI: 86.0, 91.5] were initiated on ART within 14 days of HIV diagnosis, while 26 (4.9%) [95% CI: 3.3, 7.2) participants were initiated after 14 days. A total of 32 (6.1%) [95% CI: 4.2, 8.1] participants did not start treatment following the confirmation of their HIV-positive status. For patients who missed same-day ART initiation, the median time to ART initiation was 6 days (IQR: 12 days). The timing of ART initiation following HIV diagnosis in this study is shown in Table 3.
Table 2: Clinical profiles of participants.
| Variable | Category | Frequency n (%) (N = 526) | 95% Confidence Interval |
|---|---|---|---|
| Pregnant or breastfeeding | No | 481 (91.4) | 88.7 – 93.7 |
| Yes | 45 (8.6) | 6.3 – 11.3 | |
| WHO clinical stage at diagnosis | Stage I | 350 (69.4) | 65.2 – 73.4 |
| Stage II | 66 (13.1) | 10.3 – 16.4 | |
| Stage III | 73 (14.5) | 11.5 – 17.9 | |
| Stage IV | 15 (3.0) | 1.7 – 4.9 | |
| Presence of comorbidities at diagnosis | Not present | 419 | 76.0 – 83.0 |
| Present | 107 (20.3) | 17.0 – 24.0 | |
| Comorbidities present at diagnosis | Cerebral Toxoplasmosis | 9 (8.4) | 3.9 – 15.4 |
| Meningitis | 3 (2.8) | 0.6 – 8.0 | |
| Others | 12 (11.2) | 5.9 – 18.8 | |
| Severe anemia | 8 (7.5) | 3.3 – 14.2 | |
| Tuberculosis | 75 (70.1) | 60.5 – 78.6 |
Table 3: Timing of ART initiation following HIV diagnosis.
| Variable | Category | Frequency n (%) (N = 526) | 95% CI |
|---|---|---|---|
| Lapse of time between HIV diagnosis and ART initiation | Same-day initiation | 404 (76.8) | 73.0 – 80.3 |
| Early Initiation (within 14 days of diagnosis) | 468 (89) | 9.5 – 15.3 | |
| Delayed Initiation (after 14 days of diagnosis) | 26 (4.9) | 3.3 – 7.2 | |
| Never Initiated | 32 (6.1) | 4.2 – 8.1 | |
| Median time to Initiation (IQR) days | 6 (12) |
Table 4: Socio-demographic factors affecting the timing of ART initiation following HIV diagnosis.
| Variables | Time of initiation n (%) | |||||
|---|---|---|---|---|---|---|
| Same dayn (%) | Early n (%) | Delayed n (%) | Never n (%) | P-value* | ||
| Gender | Male | 132 (75.0) | 19 (10.8) | 14 (8.0) | 11 (6.3) | 0.154 |
| Female | 271 (77.7) | 45 (12.9) | 12 (3.4) | 21 (6.0) | ||
| Pregnancy status | Pregnant | 39 (92.9) | 3 (7.1) | 0.040 | ||
| Not pregnant | 232 (75.6) | 42 (13.7) | 12 (3.9) | 21 (6.8) | ||
| Type of Population | Key pop | 17 (89.5) | 2 (10.5) | 0.415 | ||
| General pop | 387 (76.3) | 62 (12.2) | 26 (5.1) | 32 (6.3) | ||
| Place of Residence | Within CDP | 259 (78.0) | 34 (10.2) | 18 (5.4) | 21 (6.3) | 0.338 |
| Outside CDP | 145 (74.7) | 30 (15.5) | 8 (4.1) | 11 (5.7) | ||
| Age group | <10 | 7 (53.8) | 4 (30.8) | 1 (7.7) | 1 (7.7) | 0.051 |
| 10 – 19 | 13 (92.9) | 1 (7.1) | ||||
| 20 – 29 | 117 (84.8) | 10 (7.2) | 4 (2.9) | 7 (5.1) | ||
| 30 – 39 | 148 (76.7) | 23 (11.9) | 10 (5.2) | 12 (6.2) | ||
| 40 – 49 | 71 (72.4) | 15 (15.3) | 7 (7.1) | 5 (5.1) | ||
| ≥50 | 47 (68.1) | 12 (17.4) | 4 (5.8) | 6 (8.7) | ||
| Educational leve | No Formal Education | 14 (53.8) | 8 (30.8) | 3 (11.5) | 1 (3.8) | 0.036 |
| Primary | 52 (71.2) | 11 (15.1) | 4 (5.5) | 6 (8.2) | ||
| Secondary | 210 (80.2) | 26 (9.9) | 12 (4.6) | 14 (5.3) | ||
| University | 73 (80.2) | 13 (14.3) | 4 (4.4) | 1 (1.1) | ||
| Employment status | Employed | 93 (80.2) | 18 (15.5) | 5 (4.3) | 0.140 | |
| Retired | 4 (100) | |||||
| Unemployed | 295 (77.2) | 45 (11.8) | 18 (4.7) | 24 (6.3) | ||
| Marital status | Concubinage | 42 (87.5) | 6 (12.5) | 0.099 | ||
| Divorced | 7 (77.8) | 1 (11.1) | 1 (11.1) | |||
| Married | 97 (77.6) | 13 (10.4) | 8 (6.4) | 7 (5.6) | ||
| Single | 222 (75.0) | 34 (11.5) | 16 (5.4) | 24 (8.1) | ||
| Widow | 28 (71.8) | 10 (25.6) | 1 (2.6) | |||
| HIV disclosure status | Disclosed | 106 (80.3) | 17 (12.9) | 7 (5.3) | 2 (1.5) | 0.266 |
| Not disclosed | 196 (76.6) | 33 (12.9) | 12 (4.7) | 15 (5.9) | ||
*P-value comparing proportion of same-day initiation within variable categories
Socio-demographic factors affecting the timing of ART initiation following HIV diagnosis
The rate of same-day ART initiation did not differ significantly between the two sexes (P=0.154). There were 132 (75%) males initiating ART on the same day compared to 271 (77.7%) females.
The rate of same-day ART initiation was significantly higher (P=0.040) among women who were pregnant and breastfeeding at the time of HIV diagnosis 39 (92.9%) than among non-pregnant or non-breastfeeding women 232 (75.6%). Patients with at least secondary education and university education had the highest rates of same-day antiretroviral therapy initiation (80.2% in both cases) while those with no formal education had a significantly lower rate (P=0.036) of same-day initiation rate (53.8%, 14 patients).
Distance of residence from the health facility, employment status, marital status, and HIV disclosure status did not significantly affect the rate of same-day initiation the socio-demographic factors affecting the timing of ART initiation are presented in Table 4.
Clinical factors affecting the timing of ART initiation following HIV diagnosis
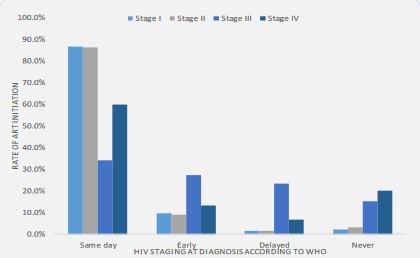
As shown in Figure 1, it was observed that patients with WHO stages I & II of the disease had significantly higher rates of same-day antiretroviral therapy initiation at 303 (86.6%) and 57(86.4%), respectively, compared to the low rates of same-day initiation observed among patients with WHO clinical stages III & IV at diagnosis at 25 (34.2%) and 9 (60.0%), respectively (P=0.001).
Trends in same-day ART initiation rates
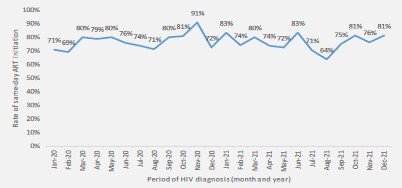
The proportion of people initiated on ART on the same day of HIV diagnosis was fairly constant in 2020. A proportion of 71% was recorded in January 2020 and 72% in December 2020. During this year, the highest rate of same-day initiation was recorded in November (91%), while the lowest rate was recorded in February (69%). A same-day initiation rate of 83% was recorded in January 2021 while a rate of 81% was recorded in December 2021. The month with the lowest rate of same-day ART initiation was August 2021 (64%). Figure 2 shows the monthly trends in same-day ART initiation rates from 2020 to 2021.
Predictors of same-day ART initiation
None of the predictors hypothesized to influence the rate of same-day ART initiation were found to be statistically significant during the multivariate analysis. However, many of them were associated with same-day ART initiation in the direction we would expect during bivariate analysis.
When all other variables were kept constant, the odds of a male patient being initiated on treatment on the same day of HIV diagnosis was 1.04 times less than the odds of a female being initiated on treatment on the same day of HIV diagnosis (AOR = 1.042[0.622-1.746]). Compared to widows, people living in concubinage were 1.4 times (1.407) more likely and people who were divorced were 1.2 times (AOR=1.243) more likely to start ART on the same day. Married individuals and those who were single were respectively 0.9 times (AOR=0.922) and 0.6 times (AOR=0.668), respectively, less likely to be initiated on treatment on the same day of HIV diagnosis. Individuals with no formal education had 65.3% (AOR=0.347) less chances of being initiated on treatment on the same day of HIV diagnosis compared to individuals who had attained tertiary education. The chances of individuals with primary education were 20.6% (AOR=0.794) less. Looking at the impact of the employment status on the timing of ART initiation following HIV diagnosis, it is observed that patients employed patients had 18.4% (AOR=1.184) more chances of being initiated on the same day of HIV diagnosis compared to unemployed ones. The chances of women who are not pregnant or breastfeeding at the time of diagnosis to start ART on the same day are 57.9% (AOR=0.421) lower than the chances of pregnant or breastfeeding women. Children aged less than 10 years were 1.2 times (AOR=1.290) more likely to be initiated on ART on the same day compared to older persons greater than 50 years of age. The adolescent age group (10-19 years) was the strongest predictor of sameday ART initiation as it was associated with the highest odds (AOR=4.482) of starting ART on the same day of HIV diagnosis. The predictors of same-day ART initiation are presented in Table 5.
Table 5: Predictors of same-day ART initiation.
| Variables | Odds ratio | Chi Square | Sig. | Adjusted odds ratio | 95% C.I for EXP(B) | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| Sex | Male | 0.041 | 0.024 | 0.876 | 1.042 | 0.622 | 1.746 |
| Pregnancy status | Not pregnant | -0.864 | 1.253 | 0.263 | 0.421 | 0.093 | 1.914 |
| Highest level of education | (Tertiary) | 5.644 | 0.130 | ||||
| No Formal Education | -1.058 | 3.011 | 0.083 | 0.347 | 0.105 | 1.147 | |
| Primary | -0.230 | 0.297 | 0.586 | 0.794 | 0.347 | 1.819 | |
| Secondary | 0.178 | 0.289 | 0.591 | 1.195 | 0.624 | 2.289 | |
| Age group | (>50) | 5.030 | 0.412 | ||||
| <10 | 0.255 | 0.107 | 0.743 | 1.290 | 0.281 | 5.919 | |
| 10-19 | 1.500 | 1.738 | 0.187 | 4.482 | 0.482 | 41.700 | |
| 20-29 | 0.917 | 3.350 | 0.067 | 2.501 | 0.937 | 6.677 | |
| 30-39 | 0.372 | 0.778 | 0.378 | 1.451 | 0.635 | 3.317 | |
| 40-49 | 0.192 | 0.214 | 0.644 | 1.211 | 0.537 | 2.729 | |
| Employment status | (unemployed) | 0.291 | 0.865 | ||||
| Employed | 0.169 | 0.291 | 0.590 | 1.184 | 0.641 | 2.187 | |
| Marital status | (widows) | 3.154 | 0.532 | ||||
| Concubinage | 0.341 | 0.289 | 0.591 | 1.407 | 0.406 | 4.877 | |
| Divorced | 0.217 | 0.057 | 0.811 | 1.243 | 0.209 | 7.387 | |
| Married | -0.081 | 0.027 | 0.869 | 0.922 | 0.352 | 2.415 | |
| Single | -0.404 | 0.663 | 0.416 | 0.668 | 0.252 | 1.766 | |
| Constant | 1.779 | 3.598 | 0.058 | 5.922 | |||
Reasons for missed same-day ART initiation from providers’ perspectives
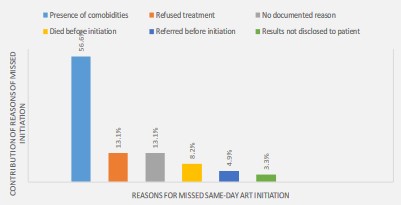
From the health care providers’ perspectives, the main documented reason for not initiating patients on the same day was the presence of comorbidities 69 (56.6%), which contraindicated ART at that time. Other reasons why patients were not placed on treatment following diagnosis included refusal by the patient to take treatment (16 (13.1%)), death before initiation (10 (8.2%)), referral to another hospital before initiation (6 (4.9%)), and the nondisclosure of results on the day of diagnosis (4 (3.3%)). We observed that 16 (13.1%) patients who were not initiated on the same day did not have any documented reason why they were not placed on treatment. Figure 3 shows the reasons for missed same-day ART initiation from healthcare providers’ perspectives.
Reasons for missed same-day ART initiation from patients’ perspectives
Of the 464 respondents, 400 (86.2%) declared they were offered treatment on the day of diagnosis, with 389 (97.3%) of them accepting it. Of the 64 (13.8%) respondents who were not offered same-day treatment, with the main reasons being their poor clinical states or the closure of the pharmacy. Eleven (2.8%) respondents who were offered same-day initiation declined treatment and advanced reasons such as doubts about their HIV statuses 6 (54.5%), side effects of drugs 2 (18.2), and the desire to discuss with their partners before taking drugs 1 (9.1%). The reasons for missed same-day ART initiation from patients’ perspectives are presented in Table 6.
Table 6: Patient’s perspectives of the reasons of missed same-day ART initiation.
| Variables | Frequency n (%) (N = 464) | |
|---|---|---|
| Patients who were offered ART on same day of diagnosis | 400 (86.2) | |
| Patients who accepted same-day initiation | 389 (97.3) | |
| Patients’ perspective of the reasons provided by the health worker for not offering drug | It was late and the pharmacy was closed | 3 (4.7) |
| It was not a working day and the pharmacy was closed | 4 (6.3) | |
| My health condition did not permit it | 51 (79.7) | |
| No reason was provided | 6 (9.4) | |
| Patients’ perspective of reasons for refusing same-day initiation | No reason | 2 (18.2) |
| Not convinced of HIV status | 6 (54.5) | |
| Scared of side effects of drugs | 2 (18.2) | |
| Wanted to discuss with partner first | 1 (9.1) |
Based on our findings, we summarized the reasons for delayed
ART initiation in Table 7.
Table 7: Grouping of the reasons for missed same-day antiretroviral therapy initiation.
| A: Patient-dependent reasons of missed same-day ART initiation |
|---|
| 1. Refusal to take treatment 2. Fear of the side effects of antiretroviral drugs 3. Presence of comorbidities such as tuberculosis that contraindicate same-day antiretroviral therapy initiation. 4. Patients’ referral to other hospitals before initiation 5. Death of patient following HIV diagnosis |
| B: Healthcare provider-dependent reasons for missed same-day ART initiation |
| 1. Circumstantial inability to disclose HIV results to patient following HIV diagnosis 2. Circumstantial inability to provide drugs to patient for various reasons |
| C: Healthcare system-dependent reasons for missed same-day ART initiation |
| 1. Closure of the pharmacy during odd hours (nights, weekends, and public holidays) |
Discussion
In this study, we assessed the effectiveness of the “test and treat” strategy in Douala, Cameroon, and established that 76.8% of patients diagnosed with HIV are placed on health care on the same day of diagnosis. This proportion increases significantly when the window of treatment initiation is increased to 14 days following diagnosis.
There are different definitions of same-day ART initiation. It could mean placing patients on ART on the day of HIV diagnosis, which is the definition we adopted in this study. It could also mean placing patients on ART on the day they become eligible for ART (for example, a patient who is diagnosed with HIV and Tuberculosis (TB) as a co-infection only becomes eligible for ART after the first two weeks of anti-tuberculosis treatment based on WHO recommendations and per the Cameroon National HIV treatment guidelines) [15,16]. There are established clinical and biological benefits to starting ART early, including significant reductions in HIV-associated morbidity and mortality [4,17]. In a study conducted by Koenig et al., the same-day HIV testing and ART initiation strategy was proven to be feasible and beneficial, as it improved retention in care with virologic suppression among patients with early-stage clinical HIV [18]. Cohen et al. concluded that early ART initiation reduced the rates of sexual transmission of HIV-1 and clinical events, indicating both personal and public health benefits of the strategy [9]. Late treatment initiation in the course of clinical HIV, on the other hand, worsens the health outcomes of individuals and can compromise the fight against the HIV/AIDS epidemic [10-12,19].
The Cameroon national treatment guidelines adopted the test-and-treat principle in 2016, and this was followed by a multiplication of sites that offer treatment to bring treatment as close as possible to the target population. However, the question of whether these amenities have favored same-day ART initiation at the Cite des Palmiers District Hospital remains to be answered. The 76.8% same-day ART initiation obtained in this study does not differ significantly from the national overall rate of linkage to ART of 84.9% reported in 2020 [20]. This shows that a majority of initiations are done on the same day of HIV diagnosis. This could be because the Cite des Palmiers District Hospital, among other hospitals in Cameroon, is supported by PEPFAR and has at its disposal facilities to rapidly exclude clinical conditions such as tuberculosis that could delay ART initiation. Also, due to the presence of HIV program staff at this hospital, pre-therapeutic sessions are highly effective and only a few patients deny treatment. The rate of SDI obtained in this study is higher than the 63.2% reported by Kerschberger et al. in Eswatini [8]. This could be because Kerschberger et al. used a larger sample size of 1,328 patients. Also, Kerschberger et al. used a nested retrospective design involving multiple centers (8 primary-care facilities and 1 secondary-care public-sector facility).
We also assessed the predictors of same-day ART initiation and determined the reasons for delayed initiation. A number of factors were found to be independently associated with a higher likelihood of same-day ART initiation, with the 10-19 years age group having the strongest association. This finding is different from the results reported by Larsen et al. who identified pregnancy as the strongest predictor of ART initiation and the study by Moon et al. who identified older age and higher levels of education as the strongest predictors of ART initiation [21,22]. This divergence could be explained by the fact that Moon et al. only considered participants who were greater than 15 years in their study while Larsen and colleagues used a larger sample size. In a survey conducted by Ndawinz et al. involving medical records of 4935 patients above 15 years of age, late ART initiation was associated with the male sex as was the case in our study [23]. However, in the study by Ndawinz et al., late ART initiation was defined as having a CD4 count of ≤100 cells/ mm3 at ART initiation whereas in our study, we defined it as initiating a patient more than 14 days after HIV diagnosis. In the current study, the odds of a male patient being initiated on treatment on the same day of HIV diagnosis were 12% less than the odds of a female patient being initiated on treatment on the same day of HIV diagnosis. Considering the educational level as a proxy for socioeconomic status, we concluded that individuals with low levels of education (no formal education or just primary education) had lower odds of being initiated on the same day than those with higher levels of education (secondary or tertiary level education). In a study conducted by Amanda et al. in Brazil in 2021, according to which compared to tertiary levels of education, incomplete basic, basic, and secondary levels of education increased the odds of late treatment initiation, similar results were obtained [24]. Similar findings were reported in Mozambique where compared with having less education, having at least secondary education was associated with a lower odds of late ART initiation among all patients [25].
In this study, 23.2% of patients were not initiated on the day of HIV diagnosis and 6.1% had not started treatment at the end of the study period. The presence of comorbidities (mainly tuberculosis), denial, fear of ARV drug side effects, and the need to discuss the HIV status with the partner before accepting treatment were reasons for the delayed ART initiation. This demonstrates the psycho-social challenges experienced by patients following HIV diagnosis and ties with the literature that shows that the complexities of drug-drug interactions, the presence of social problems, incorrect clinical or immunological staging, and the poor integration of mental health services in HIV care and treatment centers are inherently linked to delays in ART initiation [23,24,26,27].
Conclusion
The rate of same-day ART initiation in Douala is similar to the national overall rate of linkage to care, which indicates the effectiveness of the “test and treat” strategy. There was no significant independent predictor of same-day antiretroviral therapy initiation. However, factors such as age, sex, marital status, educational level, employment status, HIV disclosure status, residence, WHO clinical stage, presence of comorbidities, and pregnancy and breastfeeding statuses were associated with same-day initiation. The rate of same-day initiation was higher among females, the 10-19 years age group, pregnant and breastfeeding women, people who lived within the same health district where the HIV diagnosis was made, individuals with at least secondary education, people who had discussed their HIV-positive statuses with their partners, and individuals diagnosed with Stage I HIV. The reasons why patients are not placed on treatment on the same day of HIV diagnosis could be grouped into patient-dependent reasons, healthcare providerdependent reasons, and health system-dependent reasons. These reasons include refusal by the patient to take drugs (fovarious reasons), denial of one’s HIV status, and fear of the side effects of drugs; healthcare providers failing to provide drugs to patients either because of the presence of comorbidities or sometimes for no obvious reasons; and the non-availability of ARVs when the pharmacy is closed at night or during weekends.
Declarations
Conflict of interest statement: The authors have no conflicts of interest to declare.
Supporting information: None.
Authors’ contributions: DTE, ND, and ZF conceived and designed the study; DTE, FME, and CA wrote the first draft of the manuscript; ND and ZF analyzed the data; CA and DTE critically reviewed the manuscript. All authors approved the final version of the manuscript.
Acknowledgments: The authors thank the staff of the Cite des Palmiers Health District for their full cooperation.
Keywords: HIV/AIDS; Same-day initiation; Antiretroviral therapy; Delayed initiation; Adults; Douala.
References
- Severe P, Juste MAJ, Ambroise A, Eliacin L, Marchand C, et al. Early Versus Standard, Antiretroviral Therapy for HIV Infected Adults in Haiti. N Engl J Med. 2010; 363: 257-265.
- WHO in Cameroon Annual Report 2016-Cameroon.
- Dzudie A, Tchounga B, Ajeh R, Kouanfack C, Ebasone PV, et al. Research priorities for accelerating the achievement of three 95 HIV goals in Cameroon: a consensus statement from the Cameroon HIV Research Forum (CAM-HERO). The Pan African Medical Journal. 2021; 40.
- Guidelines for managing advanced HIV disease and rapid initiation of antiretroviral therapy.
- 90-90-90-An ambitious treatment target to help end the AIDS epidemic.
- Ford N, Migone C, Calmy A, Kerschberger B, Kanters S, et al. Benefits and risks of rapid initiation of antiretroviral therapy. AIDS. 2018; 32: 17-23.
- Ahmed I, Demissie M, Worku A, Gugsa S, Berhane Y. Effectiveness of same-day antiretroviral therapy initiation in retention outcomes among people living with human immunodeficiency virus in Ethiopia: empirical evidence. BMC Public Health. 2020; 20: 1802.
- Kerschberger B, Boulle A, Kuwengwa R, Ciglenecki I, Schomaker M. The Impact of Same-Day Antiretroviral Therapy Initiation under the World Health Organization Treat-All Policy. American Journal of Epidemiology. 2021; 190: 1519-1532.
- Cohen MS, Chen YQ, McCauley M, Gamble T, Hosseinipour MC, et al. Prevention of HIV-1 Infection with Early Antiretroviral Therapy. The New England Journal of Medicine. 2011; 365: 493.
- Ford N, Mills EJ, Egger M. Editorial Commentary: Immunodeficiency at Start of Antiretroviral Therapy: The Persistent Problem of Late Presentation to Care. Clin Infect Dis. 2015; 60: 1128-1130.
- Cescon A, Patterson S, Davey C, Ding E, Raboud JM, et al. Late initiation of combination antiretroviral therapy in Canada: a call for a national public health strategy to improve engagement in HIV care. J Int AIDS Soc. 2015; 18: 20024.
- Cesar C, Jenkins CA, Shepherd BE, Padgett D, Mejia F, et al. Incidence of virological failure and major regimen change of initial combination antiretroviral therapy in the Latin America and the Caribbean: an observational cohort study. Lancet HIV. 2015; 2: e492-500.
- Carte Sanitaire Nationale.
- White IR, Royston P, Wood AM. Multiple imputation using chained equations: Issues and guidance for practice. Stat Med. 2011; 30: 377-399.
- Rosen S, Maskew M, Fox MP, Nyoni C, Mongwenyana C, et al. Initiating Antiretroviral Therapy for HIV at a Patient’s First Clinic Visit: The RapIT Randomized Controlled Trial. PLOS Medicine. 2016; 13: e1002015.
- MacKellar D. Peer-Delivered Linkage Case Management and Same-Day ART Initiation for Men and Young Persons with HIV Infection-Eswatini, 2015-2017. MMWR Morb Mortal Wkly Rep. 2018; 67.
- The Antiretroviral Therapy Cohort Collaboration. The Changing Incidence of AIDS Events in Patients Receiving Highly Active Antiretroviral Therapy. Archives of Internal Medicine. 2005; 165: 416-423.
- Koenig SP, Dorvil N, Devieux JG, Hedt-Gauthier BL, Riviere C, Faustin M, et al. Same-day HIV testing with initiation of antiretroviral therapy versus standard care for persons living with HIV: A randomized unblinded trial. PLoS Med. 2017; 14: e1002357.
- Sobrino-Vegas P, Moreno S, Rubio R, Viciana P, Bernardino JI, et al. Impact of late presentation of HIV infection on short-, mid-and long-term mortality and causes of death in a multicenter national cohort: 2004-2013. Journal of Infection. 2016; 72: 587-596.
- Rapports d’activites -CNLS-NACC. 2016.
- Larsen A, Cheyip M, Tesfay A, Vranken P, Fomundam H, et al. Timing and Predictors of Initiation on Antiretroviral Therapy Among Newly-Diagnosed HIV-Infected Persons in South Africa. AIDS Behav. 2019; 23: 375-385.
- Moon TD, Burlison JR, Blevins M, Shepherd BE, Baptista A, et al. Enrolment and programmatic trends and predictors of antiretro-viral therapy initiation from President’s Emergency Plan for AIDS Relief (PEPFAR)-supported public HIV care and treatment sites in rural Mozambique. Int J STD AIDS. 2011; 22: 621-627.
- Ndawinz JDA, Chaix B, Koulla-Shiro S, Delaporte E, Okouda B, et al. Factors associated with late antiretroviral therapy initiation in Cameroon: a representative multilevel analysis. Journal of Anti-microbial Chemotherapy. 2013; 68: 1388-1399.
- Rodrigues A, Struchiner CJ, Coelho LE, Veloso VG, Grinsztejn B, et al. Late initiation of antiretroviral therapy: inequalities by educational level despite universal access to care and treatment. BMC Public Health. 2021; 21: 389.
- Lahuerta M, Lima J, Nuwagaba-Biribonwoha H, Okamura M, Alvim MF, et al. Factors Associated with Late Antiretroviral Therapy Initiation among Adults in Mozambique. PLOS ONE. 2012; 7: e37125.
- Feucht UD, Kinzer M, Kruger M. Reasons for Delay in Initiation of Antiretroviral Therapy in a Population of HIV-Infected South African Children. Journal of Tropical Pediatrics. 2007; 53: 398-402.
- Bracchi M, Stuart D, Castles R, Khoo S, Back D, et al. Increasing use of “party drugs” in people living with HIV on antiretrovirals: a concern for patient safety. AIDS. 2015; 29: 1585-1592.