Short Report
Volume 2, Issue 3
An Unusual Case of Neisseria Meningitidis Infection in Elderly Revealing a Primary Classic Pathway Complements Deficiency
Nadir Abdelhameed1*; Michail Kaklamanos2
1Geriatric Medicine, Guys and st Thomas’, NHS Foundation Trust, UK.
2Geriatric Medicine, East Kent Hospitals, NHS Foundation Trust, UK.
Corresponding Author :
Nadir Abdelhameed
Email: nadir.abdelhameed@nhs.net
Received : Feb 06, 2023 Accepted : Mar 20, 2023 Published : Mar 27, 2023 Archived : www.meddiscoveries.org
Citation: Abdelhameed N, Kaklamanos M. An Unusual Case of Neisseria Meningitis Infection in Elderly Revealing a Primary
Classic Pathway Complements Deficiency. Med Discoveries. 2023; 2(3): 1027.
Copyright: © 2023 Abdelhameed N. This is an open access article distributed under the Creative Commons Attribution License,
which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Primary classic pathway complement deficiencies in older people are rarely reported in the literature. The link between classical pathway complement deficiencies and Neisseria Meningitidis infections is not clearly understood. We are reporting a case of Neisseria meningitis with persistent C4 deficiency over a longer than 18-week period despite a complete clinical recovery. Uncommon infections, such as Neisseria Meningitidis infections, should prompt clinicians to consider an underlying complement deficiency.
Introduction
Complement system is a major component of the innate human immune system protecting against bacterial infections. Neisseria Meningitidis infections are primarily associated with deficiencies in the alternative and/or terminal complement pathways [1]. Complement deficiencies are rare and under-reported in older people [2]. We describe a case of N. Meningitis infection which led to the diagnosis of primary classic pathway C4 deficiency.
Case report
An 82 year old female presented to the emergency department with decreased level of consciousness and septic features. Her past medical history was suggestive of previous lichen planus, varicella zoster and basal cell carcinoma. She was febrile, hypotensive, hypoxic with GCS 12/15. On examination, she had bilateral basal crepitation, nuchal rigidity and a petechial rash of her limbs. Chest X-ray revealed bibasal consolidations. A provisional diagnosis of bilateral pneumonia with probable acute meningitis was made. Treatment with intravenous ceftriaxone and acyclovir was initiated. She had to be intubated and transferred to ITU for further management.
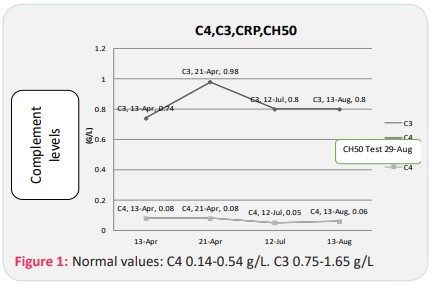
N.Meningitis type-B was isolated from both the blood cultures and CSF. Her inflammatory markers were markedly raised (Figure 1). Her renal, liver and clotting functions were normal. Low C3 and C4 complement levels were measured (Figure 1). A rheumatology screen was negative including a normal ESR. Additionally, tests for myeloma, HIV, parvovirus and hepatitis were negative. A CT chest, abdomen and pelvis also did not reveal any underlying malignancy.
She responded well to antibiotic treatment and transferred to a medical ward after three days. Twelve days later, we repeated her C3 and C4 levels, prior to discharge. C4 remained persistently low, while C3 slightly recovered (Figure 1), despite normal inflammatory markers and no signs of infection.
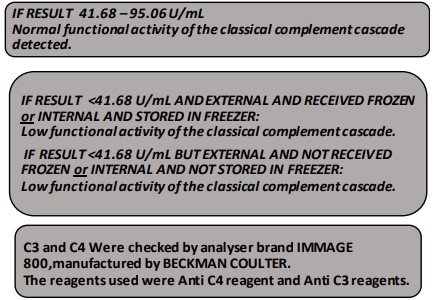
Similar results were obtained during a clinic follow up at three- and five-month interval (Figure 1). Her inflammatory markers remained within normal range and Total Complement (CH50) test confirmed low activity. We measured CRP to correlate with Compliment levels to exclude secondary causes of deficiencies and the all results post infection remission were within normal range.
CH50 BINDING SITE METHOD Used CH50 Reagent pack for use on SPLA plus, St George’s university hospital foundation trust. Immunology lab
Discussion
We hereby report the case of a patient with N.Meningitis infection causing pneumonia and acute meningitis leading to the diagnosis of primary classic pathway C4 complement deficiency. This is an unusual case, as meningococcal pneumonia is rare [3] and Neisseria meningitis is not commonly associated with classic complement deficiencies [1].
Our patient had persistently low C4 complement levels that could not be simply contributed to the acute septic phase and/ or consumption of the complement factors. We intentionally completed the CH50 test following our patient’s recovery in order to avoid any confounding risks. It is, therefore, likely that this is a case of primary C4 deficiency unmasked by the N.Meningitis infection. Co-existent immunosenescence may have contributed to this presentation. This is important as N.meningitis is mainly considered a disease of infants and adolescents/young adults [1]. However; older people have been reported to have complement deficiencies without any prior index infections [3].
Secondary C4 deficiency is less plausible mainly due to the natural course of our patient’s C4 levels up to five months after the initial infection. There was no evidence of renal or liver disease, immunosuppression, malignancy or autoimmune diseases, particularly SLE.
On discharge, meningococcal vaccination was recommended despite paucity of evidence showing clear benefits in this age group [4]. The efficacy of long-term prophylactic antibiotics has not been proven yet.
This case highlights the importance of suspecting complement deficiencies in older people presenting with uncommon infections.
Key points
• Complement deficiencies, primary or secondary, should be suspected when older people present with uncommon infections
• There is paucity of evidence related to secondary prevention of infections in this group
Conflicts of interest: The authors hereby declare that there are no conflicts of interests and that we have not received any funding in relation to this work.
References
- Botto M, Kirschfink M, Macor P, Pickering MC, Würzner R, Tedesco F. 2009 .Complement in human diseases: Lessons from complement deficiencies. Mol Immunol. 2009; 46: 2774-83
- Audemard-Verger A, Descloux E Ponard, D Deroux, A Fantin, B Fieschi, et al. Infections Revealing Complement Deficiency in Adults: A French Nationwide Study Enrolling 41 Patients. Medicine. 2016; 95: 1-4.
- Winstead JM, McKinsey DS, Tasker S, De Groote MA, Baddour LM, et al. Characterization and Review of Cases Seen Over the Past 25 Years. Clin Infect Dis. 2000; 30: 87-94.
- Cohn AC, Mac Neil JR, Clark TA, Ortega-Sanchez IR, Briere EZ, et al. Centers for Disease Control and Prevention (CDC). Prevention and Control of Meningococcal Disease: Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep. 2013; 62: 1-28.