Case Report
Volume 2, Issue 1
Successful Conservative Management of Dysfunctional Elimination Syndrome Associated with Micronutrient Deficiencies, Recurrent Juvenile Allergic Urethritis and Penoscrotal Edema
Govani DJ1; Govani ND1; Govani DR1; Panchasara NG1; Patel RR1; Midha PK2; Correia RC3; Patel RV1*
1Departments of Pediatrics and Ped Surgery, Postgraduate Institute of Child Health & Research and KT Children Govt University
Teaching Hospital, Rajkot 360001, Gujarat, India.
2J. Watumull Global Hospital & Research Centre, Delwara Road, Mount Abu, Rajasthan 307501, India.
3Santa Casa de Tatui General Hospital, 330 Maneco Pereira Road, Tatui 18273000, Sao Paulo, Brazil.
Corresponding Author :
Ramnik V Patel
Tel: 00447956896641
Fax: 00441162893395
Email: ramnik@doctors.org.uk
Received : Jan 23, 2023 Accepted : Feb 22, 2023 Published : Feb 28, 2023 Archived : www.meddiscoveries.org
Citation: Govani DJ, Govani ND, Govani DR, Panchasara NG, Patel RR, et al. Successful Conservative Management of Dysfunctional Elimination Syndrome Associated with Micronutrient Deficiencies, Recurrent Juvenile Allergic Urethritis and Penoscrotal Edema. Med Discoveries. 2023; 2(1): 1018.
Copyright: © 2023 Patel RV. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Dysfunctional elimination syndrome is a constellation of symptoms related to the urinary, genital and colorectal dysfunction of the psycho-neuro-endocrine-target organs axis origin secondary to congenital and acquired disorders characterized by functional partial silent chronic pelvic outlet obstruction in the absence of any somatic neurologic deficits. We wish to report a toddler boy with a bowel dysfunction in the form of chronic refractory constipation and voiding dysfunction leading to recurrent genital symptoms in the form of juvenile allergic urethritis, penoscrotal edema and multiple micronutrient deficiencies who was successfully managed by conservative management using biofeedback, dietary, micronutrient therapies and dysfunctional elimination bowel bladder retraining without any recurrence of symptoms.
Keywords: Allied Hirschsprung’s disorders; Bowel bladder dysfunction; Congenital colorectal secreto-motility disorders; Dysfunctional elimination syndrome; Idiopathic penoscrotal edema; Juvenile allergic urethritis; Micronutrient deficiencies; Preservative allergies; Voiding dysfunction.
Introduction
Our team has an extensive experience of dealing colorectal, genital and urinary systems with congenital and acquired problems involving anatomical diseases and functional disorders [1-7]. However, we wish to report an exciting case involving all three major output pleasure systems turning into output painful ones and implications with regards to the challenging diagnosis and subsequent successful conservative therapeutic interventions. Dysfunctional elimination syndrome (DES) is a well-known common condition in the toddler population and typically presents earlier, often after toilet training. The condition has been found to resolve after puberty in many cases possibly due to psycho-neurological and endocrinal maturity, especially the developmental and adolescent growth spurt related endocrine hormone surge. The association of the DES with micronutrient deficiencies and recurrent juvenile allergic urethritis and penoscrotal edema has not been reported.
Case report
A 4-year-old toddler boy born at term who had normal prenatal scans was delivered at term by normal spontaneous delivery. Patient was born in good condition and passed meconium and urine in the first few hours of birth. The patient had normal bowel habits in early infancy but developed chronic constipation later in infancy which was managed with intermittent laxatives and parents were advised rectal biopsy but it was refused. The patient passed meconium and urine in the first 24 hours but after few months in infancy developed chronic intermittent constipation treated with laxatives as required. Patient had severe nappy rash in neonatal and early infancy periods. During toilet training, the patient developed voiding dysfunction with urgency and frequency with intermittent voiding and dysuria at times. This symptom of constipation and recurrent lower abdominal pain and fullness were later on associated with significant pain radiating deep down in the pelvis during and after micturition, hematuria and recurrent penoscrotal edema suggestive of juvenile allergic urethritis after taking food and drinks on long shelf life associated with preservative sensitivities. Past history included infantile eczema.
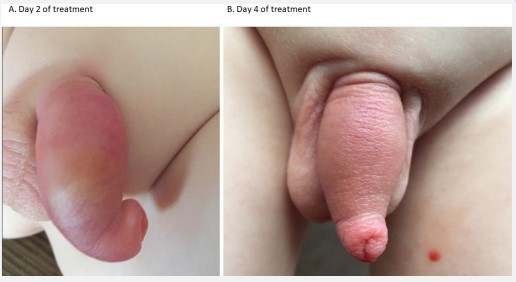
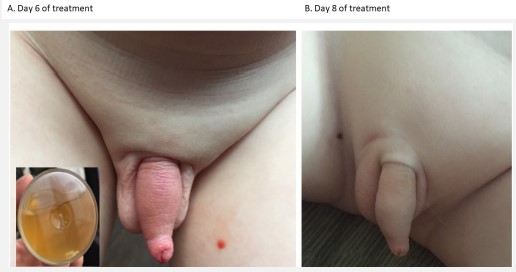
Physical examination showed pallor and signs of brittle nails with koilonychia. Abdominal examination showed rectosigmoid and left colonic severe fecal loading with tympanic note over transverse and right colon. Back examination demonstrated small tuft of hair at the bottom of spine with a shallow sacral blind ending sinus. Local genital examination depicted severe redness and swelling of the prepuce and penoscrotal area (Figure 1). Analysis of the input output charts and Bristol stool charts over the past few weeks suggested possibility of congenital colorectal secreto-motility disorder with bowel and bladder dysfunction. Bedside uroflowmetry showed prevoid volume of 300 ml with bladder scan, small volume low pressure intermittent voiding pattern and postvoid residual volume of 70 ml.
Laboratory investigations showed mixed macro and microcytic anemia with hemoglobin 108 Gm/L and normal biochemical profile. Micronutrient assay showed low levels of ferritin 15ug/L, low-normal adjusted calcium 1.97 mmol/L, low vitamin B12 92 pmol/L, folate 1.2 ug/L, and vitamin D 12 nmol/L levels.
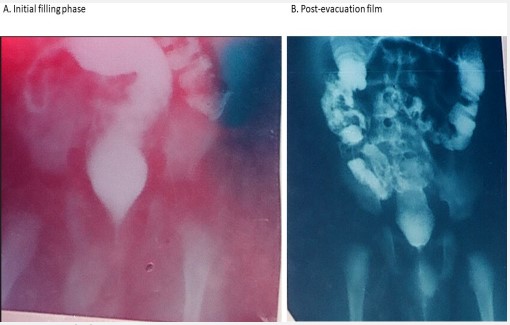
Color Doppler ultrasound scan demonstrated marked thickening of the penile and scrotal wall, with heterogeneous and edematous appearance, increased peritesticular blood flow, mild reactive hydrocele, and enlarged inguinal lymph nodes. The bladder wall was thin and the urine volume was 280 ml and the residual urine was 65 ml at first void, 35 ml at second void and 10 ml at third void. Abdominal radiograph showed gross rectosigmoid and left colonic fecal loading and excessive gas in the rest of the colon and some characterless loops in the right lower quadrant. This was confirmed by lower gastrointestinal contrast which revealed distended rectum with reversed rectosigmoid ratio (Figure 2A). The key radiological findings showed features of hypoganglionosis with gross reflux into the ileocecal reflux (Figure 2B).
In view of the worsening recurrent bowel, urinary, and genital symptoms and partial response with poor patient and parental compliance, the patient was referred to us. Avoidance of all allergens in the drinks and food, regular double or triple 2 hourly voiding and drinking liquids between 2-3 litres daily, dietary measures with balanced diet with prebiotic, probiotic, postbiotic and holobiotic therapy, micronutrient therapy, evacuation of colorectal loading to remove the reservoir of microbes and hydrodistension of the left colon by increasing water and fibre content to reduce the incidence and severity of ileocecal reflux and associated small intestinal bacterial overgrowth by using Movicol deimpaction regime initially followed maintenance regime with regular laxatives to keep stools soft and formed, biofeedback comprehensive therapy, behavioural therapy, balance between exercise and, pelvic muscle relaxation techniques, meditation, relaxing music therapy were all implemented without any resort to topical or systemic steroids.
Patient responded well to the treatment due to well-coordinated and executed plan by patient and parents at home, teachers and nurse at school and at biofeedback therapy by the experts. In one week, all the bowel, bladder and genital symptoms and signs got reversed completely (Figures 1,3,4). At last, follow up 5 years after the treatment, the patient is completely asymptomatic, growing well and having normal development with very good self esteem and securing high grades with patient, parents, teachers and local professionals are all happy with the results.
Discussion
In most children with elimination syndrome, the symptoms are mild to moderate and usually improve with advancing age. Occasionally a sever variant especially with acquired risk factors may prove refractory with worsening symptoms and failing medical management [1]. These disorders are more common in females and associated with a higher incidence of urinary and genital tract symptoms but this is the first case of a male patient with triple colorectal, urinary and genital tract recurrent symptoms being treated successfully by conservative management.
In the elimination syndrome, the precise pathophysiology involves functional obstruction to bowel, bladder and urethral sphincter in-coordination with urethro-ejaculatory redux into the seminal vesicles, prostate and vas deferens and may simulate acute scrotum [4-7]. The bowel dysfunction appears to be the primary, bladder secondary and genital tract functional obstruction seems to be tertiary as the chronology of symptoms suggests in this patient.
The bowel congenital followed by acquired dysfunctional disorders are a heterogenous group of functional disorders, are a group of allied Hirschsprung’s disorders (AHA) or variants of Hirschsprung's disorders. They clinically resemble Hirschsprung's disease (HD), despite the presence of ganglion cells in rectal suction biopsies and require specific histological, immunohistochemical and electron microscopic investigations to diagnose them. They include intestinal neuronal dysplasia, intestinal ganglioneuromatosis, isolated hypoganglionosis, immature ganglia, absence of the argyrophil plexus, internal anal sphincter achalasia and congenital smooth muscle cell disorders, malformations of the muscularis propria, degenerative leiomyopathy, leiomyositis, and mitochondriopathies [8,9].
The congenital colorectal motility disorders of their own may remain silent. However, certain additional acquired risk factors during psychological stress to the fetus, infant or child may come into play. During stress the flight or fight mode is on and the neurological imbalance between the sympathetic and parasympathetic nervous system may lead to manifest it clinically [1,2]. In addition, especially during growth spurts with certain hormones. in coordination between involuntary internal sphincter and voluntary pelvic sphincter muscles in the bowel, bladder and genital regions. may lead to increased resistance. This evacuates the contents with retention and reservoir function with associated increased risk of growth and development of resistant microbes and lead to back pressure with reflux into the ileocecal valve, vesicoureteral reflux or retrograde flow into the ejaculatory ducts, prostate and vas deferens tubes into the epididymis and testis with subsequent presentation as an acute scrotum [4-7]. It is understood to be an abnormal, learned response to uncontrolled bowel, bladder or urethral contractions which usually develops early in life.
Micronutrient deficiencies following ileocecal reflux and small intestinal bacterial overgrowth is well known despite anatomical intact small bowel as the functional loss leads to several micronutrient deficiencies [3]. The primary hind gut dysfunction causing ileocecal reflux leads to terminal ileal content absorption of vitamin b12 and folate poor and difficult as secondary midgut effects. While hind gut acting on the duodenojejunal flexure may lead to partial duodenal obstruction and gastric outlet obstruction secondarily leading to stagnation and inflammation affecting absorption of the micronutrients like iron and calcium hampered from the C loop of the duodenum. The tertiary effects are seen with bile reflux into the stomach and gastritis and gastroesophageal reflux disease allowing less intake of food thereby causing or potentiating the low micronutrient levels observed in these patients [3].
Association between micronutrient levels and allergies in the form of chronic spontaneous urticaria has been established [10]. Multiple micronutrient deficiencies have been found in association of the various skin allergies [11]. Ameliorating atopy by compensating micronutritional deficiencies in immune cells have been shown to be effective so is the vitamin D supplementation [12,13]. We strongly believe that the primary colorectal secreto-motility disorders provides a solid foundation under favourable circumstances in some patients to secondarily affect the midgut to cause malabsorption and small intestinal bacterial overgrowth and tertiarily cause foregut symptoms which may be the peak of the iceberg and apparently it may appear that associated foregut symptoms are the real culprit as evident from recent observation that most dermatological allergic conditions have associated gastrointestinal symptoms in majority of these patients [14]. The micronutrient deficiencies can predispose or exacerbate the juvenile urethral and penoscrotal skin allergies due to preservative sensitivities the metabolites of which are excreted in the urine so affecting these urogenital structures primarily and enthusiastically treated them with steroids at least in short term to get rid of the symptoms in association with avoidance of the allergen/s [4-7]. Now with this evidence we have stopped treating juvenile or adolescent allergic urethritis with topical and/or systemic steroids and avoidance of allergen with targeting primary risk factors to permanently treat this new condition.
This hitherto unreported observation of the triple pelvic outlet functional obstruction in a male child involving three of the major body systems alerts us to the need to carefully take detailed history from prenatal period to the current circumstances, examine the input and output diary critically, uroflowmetry, ultrasound, and evaluating all the risk factors together with any abnormal or grey zone clinical and investigative findings in such cases [1]. Increasing fecal retention may be the primary problem providing reservoir of the resistant microbial flora on one hand compressing other pelvic structures and secondarily affecting urinary tract by repeated voiding dysfunction, allergies and genital tract is active at adolescent age onwards and can affect it tertiarily.
Conclusion
In conclusion we believe that the series of risk factors led to the delay in the accurate diagnosis and once the underlying pathophysiology was clearly explained; the team worked so well and implemented it vigorously with very good functional recovery of the bowel, bladder and genital dysfunctions. Identifying and reporting these unusual cases is essential to further expand our understanding of these conditions and their potential associations. These cases illustrate the anatomic spectrum of variants of autonomic innervations of these systems as well as support intermittent spontaneous recovery of the symptoms when the circumstances being favourable thereby confusing the patient, parents, professionals and public alike thinking that the patient being nearly normal at times and have worsening symptoms especially during taxing times of the major pubertal growth spurts when they have almost used all their reserves on one hand the body growth demands goes up sharply. The professionals having knowledge, training, qualifications and experience in pediatric, surgical, urological and gynecological fields with broad spectrum coverage may be more beneficial than single system specialist to holistically and comprehensively evaluate such complex case effectively with minimum risk and maximum returns. Recurrent and refractory nature of presentations should alert the clinician about the possibility of underlying silent underground colorectal secreto-motility disorder as possible primary problem and detailed investigations by experienced team may yield promising excellent prognosis.
Declarations
Acknowledgments: We are grateful to Dr. Jitendra G Govani Primary Care Physician and Dr Anilkumar Trambadia MD, DCH and Dr Kavita Govani MD, DCH Consultant Neonatologists and Paediatricians for initial referral and subsequent local follow up of this case.
Conflict of interest: The authors have no conflict of interest to declare. No funding source was involved in this study.
Ethical approval: All procedures performed on human participants were in accordance with the ethical standards of the institutional and national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from the parents and all the relatives involved prior to all the procedures. Parents and all involved parties were informed about the various diagnostic and therapeutic procedures.
References
- Govani DJ, Govani ND, Govani DR, Panchasara NG, Patel RR, Midha PK, et al. Successful Conservative Management of Triple Pelvic Outlet Functional Obstruction Syndrome with Voiding, Menstrual and Bowel Dysfunctions in an Adolescent Girl with long term follow up. J Urol Neph St 4(2)-425-31 2023. JUNS. MS.ID.000181. DOI: 10.32474/JUNS.2023.04.000181.
- Govani DJ, Trambadia, RA, Chhaniara RA, Mirani ZR, Chhaniara AP, Midha PK, et al. Pre-Operative Diagnosis of Infantile Triad of Waugh’s Syndrome Associated with-Hypoganglionosis-Key Radiological Findings. Health Child Pediatr SMP. 2023, 1; 1-9.
- Govani DJ, Trambadia RA, Chhaniara RA, Mirani ZR, Corracia RC Midha PK, et al. “Is anemia frequently recognized in gastroschisis compared to omphalocele? A multicenter retrospective study in southern Japan” by Sugita, K et al Ped Surg Intl 39(1):26, 2022, Submission ID 275f1188-27e3-472d-8c80-85f57a1cd539, DOI: 10.1007/s00383-022-05288-8
- Patel RV, Brimioulle M, Govani D, Youssef T. Juvenile allergic urethritis with urethro-ejaculatory reflux presenting as acute intermittent bilateral testicular torsion. BMJ Case Rep. 2015; 2015: ii: bcr2014207392.
- Goring J, Patel R, Asharaf J, Gopal M, Subramaniam R. Experience with instillation of triamcinolone into the urethra for idiopathic urethritis. Absracts for 23th Congress of the European Society for paediatric urology. ESPU, Genova, Italy. 2013; 225.
- Ninan GK, Pringle K, Patel RV. Upper urinary tract inflammation and dilatation secondary to idiopathic urethritis- a plea for steroid treatment. Int J Urol. 2014; 21(3): 348-9.
- Ninan GK, Bhishma P, Patel R. Steroid Treatment for Recurrent Epididymitis Secondary to Idiopathic Urethritis and Urethrovasal Reflux. Eur J Pediatr Surg Rep. 2013; 1: 56-59.
- Friedmacher F, Puri P. Classification and diagnostic criteria of variants of Hirschsprung’s disease. Pediatr Surg Int. 2013; 29(9): 855-72.
- Muto M, Matsufuji H, Taguchi T, Tomomasa T, Nio M, Tamai H, et al. Japanese clinical practice guidelines for allied disorders of Hirschsprung’s disease. Pediatr Int. 2018; 60(5): 400-410.
- Wu CH, Eren E, Ardern-Jones MR, Venter C. Association between Micronutrient Levels and Chronic Spontaneous Urticaria. Biomed Res Int. 2015; 2015: 926167.
- Wu CH, Eren E, Ardern-Jones MR, Venter C. Association between Micronutrient Levels and Chronic Spontaneous Urticaria. Biomed Res Int. 2015; 2015: 926167.
- Bartosik T, Jensen SA, Afify SM, Bianchini R, Hufnagl K, Hofstetter G, et al. Ameliorating Atopy by Compensating Micronutritional Deficiencies in Immune Cells: A Double-Blind PlaceboControlled Pilot Study. J Allergy Clin Immunol Pract. 2022; 10(7): 1889-1902.e9.
- Tuchinda P, Kulthanan K, Chularojanamontri L, Arunkajohnsak S, Sriussadaporn S. Relationship between vitamin D and chronic spontaneous urticaria: a systematic review. Clin Transl Allergy. 2018; 8: 51.
- Armin Abadeh, Sari M Herman, Rupert Abdalian et al. The prevalence of gastrointestinal symptoms and cobalamin deficiency in patients with chronic urticaria. 07 June 2022, PREPRINT (Version 1) available at Research Square.